Recurrence Of Ptc After Optimized Surgery
Having considered in detail the disease PTC, aspects of optimized surgery for this disease, and different forms and implications of disease recurrence, a coherent management plan can be synthesized.
As evidence in support of this approach, the results are presented of the Mayo Clinic moderate surgical approach including preoperative US for detection and mapping of LNM NTTx or TTx routine C-VI CLND, and lateral internal jugular lymph node dissection when indicated by either positive nodes detected by palpation or US. From 1999-2006, 420 patients were treated with this comprehensive approach, and excluded only the few patients who were found intraoperatively to be unresectable. Tumors were multicentric in 40%, averaged 1.7 cm in size, were bilateral in 30%, demonstrated extrathyroidal extension in 17%, were associated with C-VI LNM in 51% and lateral LNMs in 20%, and had MACIS low-risk prognostic scores in 84%. RAI was used in 40% of patients. Relapse of LNM occurred in previously operated fields in 5% of patients 3% had true local recurrence or distant metastasis, with complications limited to 1.2% hypoparathyroidism and only a single patient suffered unintentional RLN paralysis. Only a single patient had died as a direct result of PTC at last follow-up.
Shift Of Emphasis: Disease
Reassuringly, however, in a meta-analysis of 23 studies regarding the use of RAI for PTC, the 10-year disease-specific mortality remained extremely low at about 1.7% . With the new fixation of concern on lymph node relapse, the new ability to uncover even tiny amounts of disease during the course of compulsive postoperative disease surveillance, consequent liberal use of RAI to ablate this modest disease, the fear on the part of physicians and patients alike that even miniscule amounts of cancer was extremely worrisome and required intervention, surgeons felt the obvious impetus to minimize any potential disease relapse at the time of surgery. Disease relapse occurs in three important forms: distant disease, true local recurrence , and lymph nodes. While the first two are evidence of biologically aggressive disease that may eventually be life-threatening, they are distinctly uncommon in most consecutive series of PTCconsistent with the known very low disease-specific mortality of PTC. However, about 90% of PTC disease relapse is LNM. These LNM are the usual culprits identified during postoperative surveillance, and, therefore, have been the focus of considerable study and debate over the prior 15 years.
Life After Thyroid Cancer Surgery #2 Thyroid Hormone Supplements
Depending of the type of thyroid cancer surgery you have, you could need thyroid hormone medication. There are numerous formulations and types, but all these medications do a great job at replacing or supplementing the natural hormone your thyroid makes. Low risk thyroid cancers in patients who only have half of their thyroid removed do not need aggressive thyroid hormone suppression . Many patients who have half of their thyroid removed do not need thyroid hormone supplementation at all. The healthy remaining half of their thyroid makes enough hormone in many instances. If half of your thyroid was removed during your thyroid cancer surgery, you will routinely get your thyroid hormone levels checked to make sure the remaining half of thyroid is making enough thyroid hormone.
Recommended Reading: How To Fix Hair Loss From Thyroid
Outlook For Thyroid Cancer
Around 9 in every 10 people are alive 5 years after a diagnosis of thyroid cancer. Many of these are cured and will have a normal lifespan.
But the outlook varies depending on the type of thyroid cancer and how early it was diagnosed. At present the outlook is:
- more than 9 in 10 people with papillary carcinoma live at least 5 years after diagnosis
- more than 9 in 10 people with follicular carcinoma live at least 5 years after diagnosis
- more than 7 in 10 men, and around 9 in 10 women with medullary thyroid carcinoma live at least 5 years after diagnosis
- around 1 in 10 people with anaplastic thyroid carcinoma live at least 5 years after diagnosis
Up to 1 in 4 people treated for thyroid cancer are later diagnosed with cancer in another part of the body, such as the lungs or bones, but cancer can often be treated again if this happens.
Page last reviewed: 28 August 2019 Next review due: 28 August 2022
Keeping Personal Health Records
You and your doctor should work together to develop a personalized follow-up care plan. Be sure to discuss any concerns you have about your future physical or emotional health. ASCO offers forms to help keep track of the cancer treatment you received and develop a survivorship care plan when treatment is completed.
This is also a good time to talk with your doctor about who will lead your follow-up care. Some survivors continue to see their oncologist or endocrinologist, while others transition back to the care of their primary care doctor or another health care professional. This decision depends on several factors, including the type and stage of cancer, side effects, health insurance rules, and your personal preferences.
If a doctor who was not directly involved in your cancer care will lead your follow-up care, be sure to share your cancer treatment summary and survivorship care plan forms with them, and with all future health care providers. Details about your cancer treatment are very valuable to the health care professionals who will care for you throughout your lifetime.
The next section in this guide is Survivorship. It describes how to cope with challenges in everyday life after a cancer diagnosis. Use the menu to choose a different section to read in this guide.
Also Check: Everlywell At-home Thyroid Test
Keeping Health Insurance And Copies Of Your Medical Records
Even after treatment, its very important to keep health insurance. Tests and doctor visits cost a lot, and even though no one wants to think of their cancer coming back, this could happen.
At some point after your cancer treatment, you might find yourself seeing a new doctor who doesnt know about your medical history. Its important to keep copies of your medical records to give your new doctor the details of your diagnosis and treatment. Learn more in Keeping Copies of Important Medical Records.
Life After Thyroid Cancer Surgery #1 Quality Of Life Expectations
Life after thyroid cancer surgery can be tough and worrisome, especially early on. You should not fret about the recovery or thyroid hormone medication. If your thyroid cancer surgery is done at an expert center such as ours, the complication rates are extremely low, and almost everyone recovers quickly and without issue or permanent problems . Your quality of life is very unlikely to be negatively affected by thyroid cancer surgery done correctly in the hands of experts.
Learn more about finding the best thyroid cancer surgeon here.
Finally, there is a lot of misinformation causing worry about being on thyroid medication, particularly about weight gain and fatigue. Thyroid hormone medication and diligent follow-up regarding the dosage and your thyroid hormone levels is critical after your thyroid cancer surgery. As long as the patient is compliant with the necessary medication and follow-up, then their thyroid levels should be appropriate. If your thyroid levels are where they should be, then thyroid medication or thyroid cancer surgery will NOT be the cause of weight gain, fatigue, hair loss, etc. that everyone is concerned about. The reality is, almost everyone on thyroid hormone medication will do great as long as they take the medication as directed, get their thyroid levels checked 1-2 times yearly at a minimum, and maintain a healthy lifestyle. Thyroid hormone medication is very unlikely to cause symptoms, side effects, or a change in your quality of life.
Also Check: Papillary Thyroid Cancer Recurrence In Lymph Nodes
What Is Papillary Thyroid Carcinoma
Papillary thyroid carcinoma is the most common type of cancer to affect your thyroid — a butterfly-shaped gland that sits just below your voice box. It’s only about as big as a quarter, but the hormones it makes help control how your body works, including your blood pressure, heart rate, and temperature.
While it may come as a shock to learn you have papillary thyroid carcinoma, keep in mind that it’s a slow-growing cancer that usually can be cured.
Will I Need Follow
Yes. At first, you’ll get blood tests every few months to check your thyroid hormone levels and get the dose right for your medicine.
Once everything has evened out, you’ll get an ultrasound and blood tests every 6-12 months. This is to check that you still have the right dose for your meds and to make sure the cancer hasn’t come back.
Show Sources
Read Also: Fine Needle Aspiration Of Thyroid
Small Papillary Thyroid Cancer Is Not Without Risk
Newswise Patients with micropapillary thyroid cancersmall tumors equal to or less than 1 centimeterand tumors even smaller, less than 1 millimeter are more common and not without a risk as previously thought, according to a new study presented on Fri., Oct. 5, at the 78th Annual Meeting of the American Thyroid Association in New York.
This is contrary to the widely perceived belief that small papillary thyroid cancers are clinically insignificant and don’t require active treatment. Papillary is the most common type of thyroid cancer, accounting for about 80% of all thyroid cancers.
The findings suggest that the size of the tumor itself may not be the sole determinant for the degree of the cancer’s aggressiveness. Small papillary cancer can indeed metastasize or spread to other parts of the body. Ten percent of patients in the study with micropapillary cancer and six percent of those with less than 1 mm cancers had tumors that spread to nearby lymph nodes in the neck.
Researchers also found that a substantial proportion of patients in their study had micropapillary and less than 1 mm thyroid cancers, suggesting that small papillary cancers are quite common. Close to half of papillary thyroid cancer patients in the study had micropapillary cancer, while over a quarter of these patients had less than 1 mm cancer.
Use Of Radioactive Iodine And Papillary Thyroid Cancer
Thyroid cells are unique in that they have the cellular mechanism to absorb iodine. The iodine is used by thyroid cells to make thyroid hormone. No other cell in the body can absorb or concentrate iodine in a similar fashion than does the thyroid. Physicians can take advantage of this fact and give radioactive iodine to patients as a treatment option for papillary thyroid cancer. The use of iodine as a cancer therapy was the first targeted therapy ever developed for any type of human cancer.
There are several types of radioactive iodine, with one type being highly toxic to cells. Papillary thyroid cancer cells absorb iodine therefore, they can be destroyed by giving the toxic isotope . Again, not everyone with papillary thyroid cancer needs this treatment, but those with larger tumors, tumors that have spread to lymph nodes or other areas including distant sites, tumors that are aggressive microscopically may benefit from this treatment.
Radioactive iodine therapy is particularly effective in children with thyroid cancer which has spread extensively to lymph nodes and even to distant sites in the body such as the lungs. Although in theory, radioactive iodine is a very attractive treatment approach for papillary thyroid cancer, its use has decreased over the years except for the specific indications as described above.
Recommended Reading: Where Can I Get Tested For Thyroid Problems
How Is Papillary Thyroid Cancer Diagnosed
Papillary thyroid cancer usually presents as a lump or nodule on your thyroid gland. You may notice it, or your healthcare provider may discover it during a routine neck examination. Sometimes, the nodule is discovered incidentally by imaging tests you get for other medical reasons.
Your healthcare provider will likely order the following tests to help diagnose PTC:
- Imaging tests: Your provider may order imaging tests to identify the nodule on your thyroid. These tests might include thyroid ultrasound, CT scan and/or magnetic resonance imaging .
- Fine needle aspiration : Your provider will likely want to take a small tissue sample, called a biopsy, from the nodule on your thyroid using a very thin needle. A pathologist will look at the tissue under a microscope to see if there are cancer cells and, if so, what type of thyroid cancer it is.
Your healthcare provider may also recommend genetic counseling to see if you have a genetic condition that may have caused PTC and may cause other types of tumors.
Papillary Thyroid Cancer: Who Gets It

Papillary thyroid cancer can occur in people of all ages from early childhood to advanced ages although it is most common in people between age 30 and 50. Papillary thyroid cancer affects women more commonly than men, and it is most common in young women. Thyroid cancer is now the fifth most common malignancy among women in the United States. Since it can occur at any age, everybody should be aware of any changes in their thyroid gland and make sure their doctor feels the thyroid gland when getting a routine check-up. For more details on who gets papillary thyroid cancer, the increasing incidence, and ages of patients affected, go to our page on the Incidence of Papillary Thyroid Cancer.
Also Check: Thyroid And Adrenal Support Supplements
How Common Is Thyroid Cancer
Thyroid cancer is a rare form of cancer, accounting for less than 1% of all cancer cases in the UK.
It’s most common in people aged 35 to 39 years and in those aged 70 years or over.
Women are 2 to 3 times more likely to develop thyroid cancer than men. It’s unclear why this is, but it may be a result of the hormonal changes associated with the female reproductive system.
Can I Lower The Risk Of My Cancer Progressing Or Coming Back
If you have thyroid cancer, you probably want to know if there are things you can do that might lower your risk of the cancer growing or coming back, such as exercising, eating a certain type of diet, or taking nutritional supplements. Unfortunately, its not yet clear if there are things you can do that will help.
Adopting healthy behaviors such as not smoking, eating well, getting regular physical activity, and staying at a healthy weight is important. We know that these types of changes can have positive effects on your health that can extend beyond your risk of cancer.
Read Also: Dry Flaky Eyelids And Thyroid
How Is It Treated
If the cancer is very small, your doctor may suggest you just keep an eye on it with regular ultrasounds. When you do need treatment, it’ll likely go like this:
Surgery. In most cases, your doctor removes the entire thyroid, along with any lymph nodes that look to be problems.
If the cancer is small, you might choose to have only part of your thyroid removed. Even in this case though, many doctors think it’s better to take it out completely. It can make follow-up care work better and lower the chances that cancer comes back.
Radioactive iodine ablation. Surgery alone may cure the cancer, so not everyone needs this step. After the operation, your thyroid gets tested. The results will help you and your doctor decide if you might need RAI ablation to keep cancer from returning.
This is typically a one-time treatment where you take a pill with radioactive iodine. Any leftover thyroid cells take in the iodine, which then kills them. It doesn’t usually have side effects, since only thyroid cells soak it up.
You typically get RAI ablation if you had nodules bigger than 4 centimeters or if the cancer:
- Grows beyond the thyroid
- Moves into the lymph nodes
- Spreads to another part of your body
Thyroid hormone pills. You start taking these after surgery. It gives your body the thyroid hormones that you no longer make on your own, since your thyroid has been removed. You’ll typically take one pill a day for the rest of your life.
Papillary Thyroid Cancer: What About Lymph Nodes
We have lymph nodes all over our body that are made up of groups of infection-fighting and cancer-fighting immune cells. We all have had “swollen glands” in our neck when we had a sore throat or tonsils. These same glands that get swollen when we have a neck infection can help fight cancer by preventing the cancer cells from spreading from the thyroid to the rest of the body. It is common for papillary thyroid cancer to spread into the lymph nodes of the neck before the cancer is discovered and diagnosed. Again, since there usually aren’t any symptoms, the cancer grows slowly for years and has time to spread into the lymph nodes, which are doing their job of capturing the cancerous cells before they can spread further. Thus, cancer that has spread into the neck lymph nodes is common with papillary thyroid cancer and may occur in as many as 40 percent of patients with small papillary cancers. In patients with larger papillary thyroid cancers, lymph node spread within the neck lymph nodes may occur in up to 75 percent of cases.
Read Also: Natural Cures For Thyroid Disorders
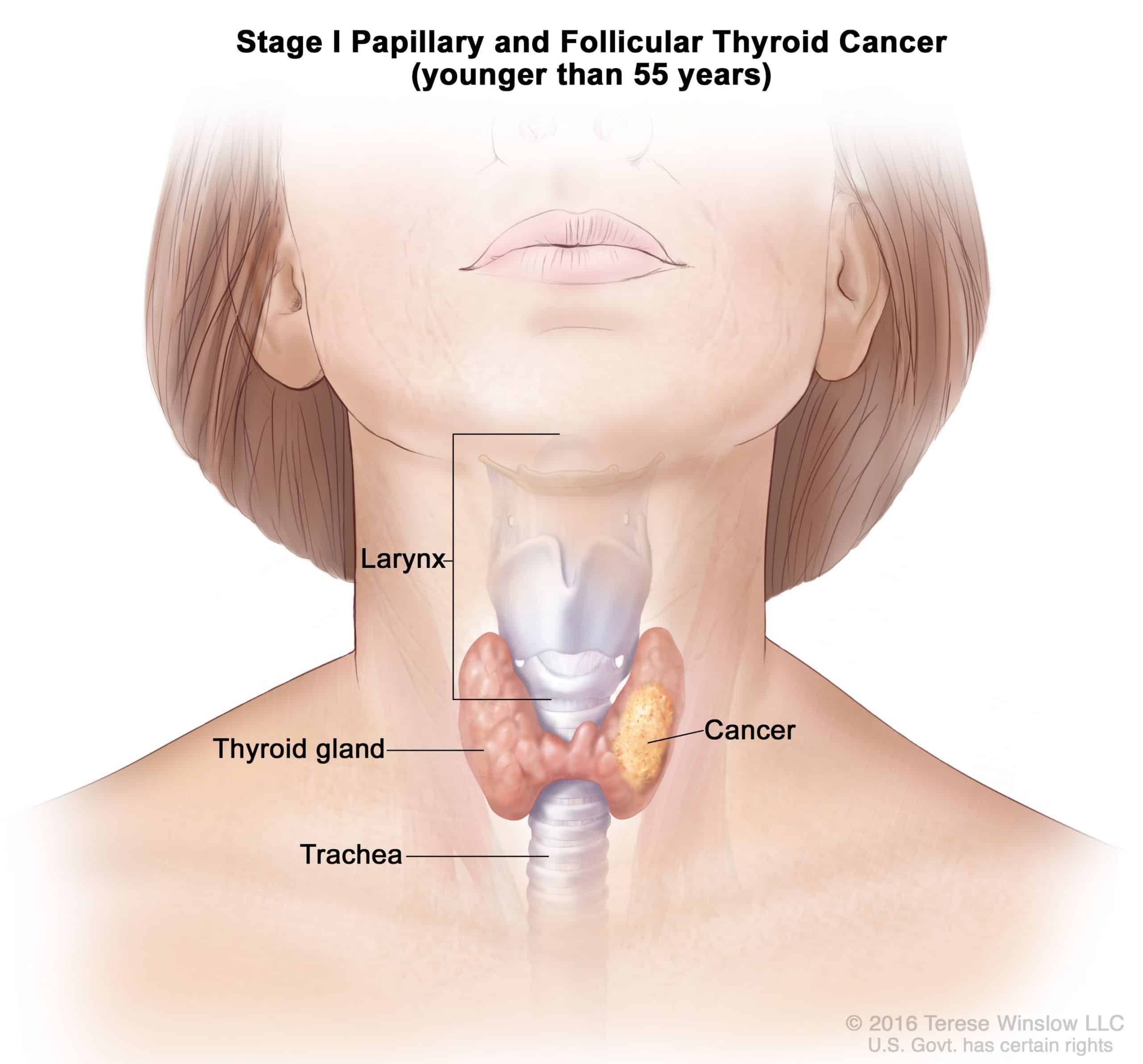
Tnm System For Thyroid Cancer
Cancer staging describes how large a cancer is, and the degree to which the disease has spread. The staging guidelines developed by the American Joint Committee on Cancer are often used to stage thyroid cancers. The stages are based on three categories:
T : This describes the primary tumor size.
N : This indicates whether the thyroid cancer cells have spread to regional lymph nodes.
M : This refers to whether the cancer has metastasized .
Recurrence Of Thyroid Cancer
Although thyroid cancer recurrence is not common, there are many treatment options available if it happens. If a cancer recurrence is detected in the neck lymph nodes, the best course of action is usually an operation to remove the affected node or additional treatment with RAI ablation. In order to determine the best treatment for recurrent thyroid cancer, it is critical to work with an experienced team of thyroid specialists.
You May Like: Hair Loss With Thyroid Medication