When Should I See My Healthcare Provider About Papillary Thyroid Cancer
If youve been diagnosed with papillary thyroid cancer, youll need to see your healthcare team regularly to monitor your treatment progress. Youll also need long-term monitoring every six to 12 months to look for cancer recurrence for at least five years.
If you had your thyroid removed and/or had radioactive iodine therapy as part of treatment, youll need to take thyroid hormone medication for the rest of your life. Your healthcare provider will want to monitor your thyroid hormone levels throughout your life to make sure your medication dosage is working for you.
A note from Cleveland Clinic
Receiving a cancer diagnosis is unsettling, regardless of the type. The good news is that papillary thyroid cancer often has an excellent prognosis. Your healthcare team will work with you to determine the best treatment plan for you.
Last reviewed by a Cleveland Clinic medical professional on 06/28/2022.
References
Characteristics Of Papillary Thyroid Cancer
-
Peak onset ages are 30 to 50 years old.
-
Papillary thyroid cancer is more common in females than in males by a 3:1 ratio.
-
The prognosis is directly related to tumor size. Less than 1.5 cm is a good prognosis.
-
The prognosis is also directly related to age. Patients under 55 years of age do much better than patients who are over 55 years of age.
-
The prognosis is directly related to gender. Women have a much better prognosis than do similarly aged men.
-
This cancer accounts for 85% of thyroid cancers due to .
-
In more than 50% of cases, it spreads to lymph nodes of the neck.
-
Distant spread is uncommon.
-
The overall cure rate is very high .Management of Papillary Thyroid Cancer
Considerable controversy exists when discussing the management of well-differentiated thyroid carcinomas both papillary thyroid cancer and even follicular thyroid cancer.
Some experts contend that if these tumors are small and not invading other tissues then simply removing the lobe of the thyroid that harbors the tumor will provide as good a chance of cure as removing the entire thyroid.
These proponents of conservative surgical therapy relate the low rate of clinical tumor recurrence despite the fact that small amounts of tumor cells can be found in up to 88% of the opposite lobe thyroid tissues. They also cite some studies showing an increased risk of and recurrent laryngeal nerve injury in patients undergoing total thyroidectomy .
Tnm System For Thyroid Cancer
Cancer staging describes how large a cancer is, and the degree to which the disease has spread. The staging guidelines developed by the American Joint Committee on Cancer are often used to stage thyroid cancers. The stages are based on three categories:
T : This describes the primary tumor size.
N : This indicates whether the thyroid cancer cells have spread to regional lymph nodes.
M : This refers to whether the cancer has metastasized .
Read Also: How To Test For Overactive Thyroid
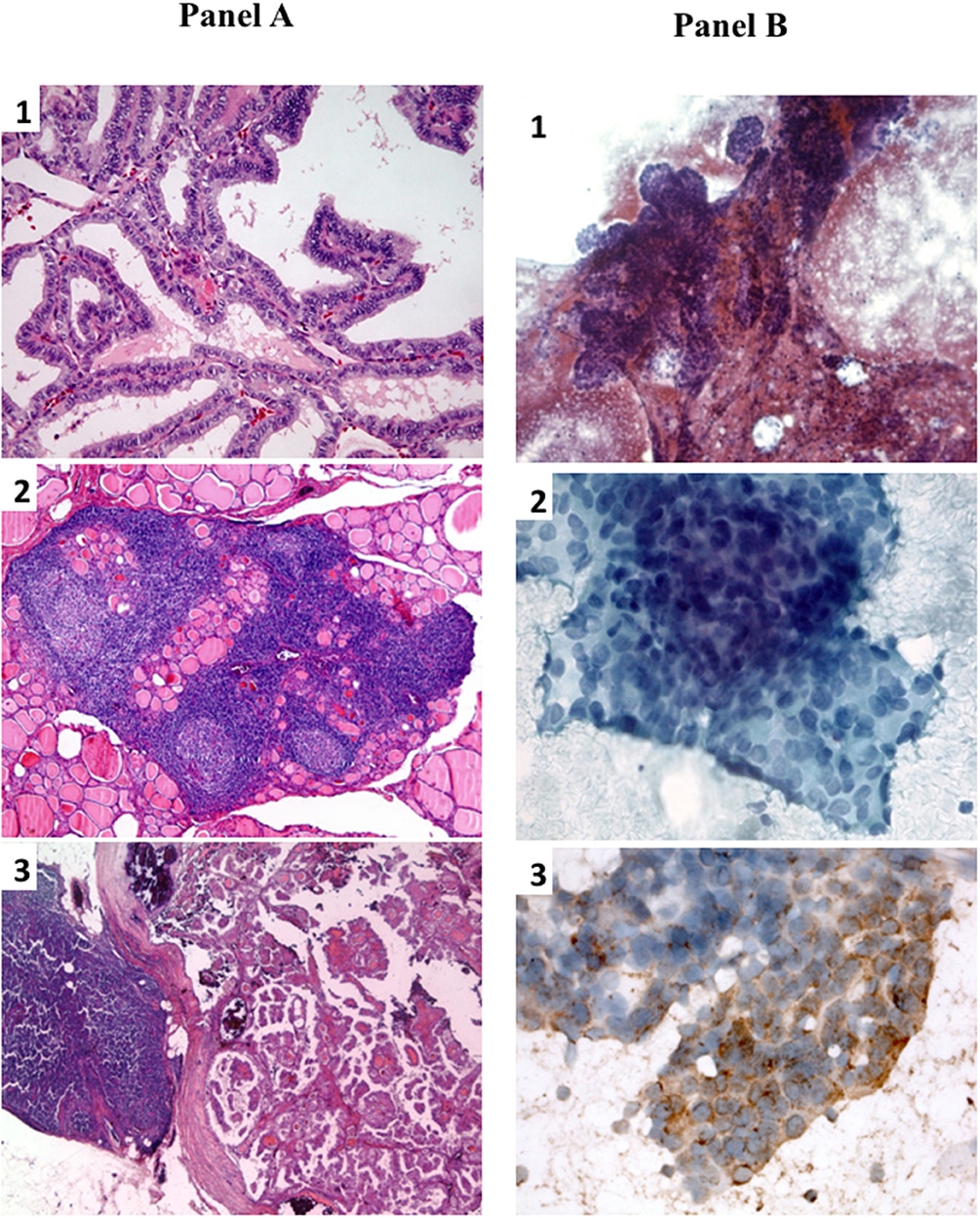
Papillary Cancer And Its Variants
Most cancers are treated with removal of the thyroid gland , although small tumors that have not spread outside the thyroid gland may be treated by just removing the side of the thyroid containing the tumor . If lymph nodes are enlarged or show signs of cancer spread, they will be removed as well.
In addition, recent studies have suggested that people with micro-papillary cancers may safely choose to be watched closely with routine ultrasounds rather than have immediate surgery.
Even if the lymph nodes arent enlarged, some doctors recommend central compartment neck dissection along with removal of the thyroid. Although this operation has not been shown to improve cancer survival, it might lower the risk of cancer coming back in the neck area. Because removing the lymph nodes allows them to be checked for cancer, this surgery also makes it easier to accurately stage the cancer. If cancer has spread to other neck lymph nodes, a modified radical neck dissection is often done.
Treatment after surgery depends on the stage of the cancer:
People who have had a thyroidectomy will need to take daily thyroid hormone pills. If RAI treatment is planned, the start of thyroid hormone therapy may be delayed until the treatment is finished .
Multivariate Analyses According To Recurrence
We divided the number of positive LN and LN ratio to avoid the interference in nodal factors. Multivariate Cox-proportional hazards regression analyses revealed that LN ratio> 5 was a predictor of recurrence in model I , and that gross ETE and positive LN more than 3 were predictors of recurrence in model II .
Table 3 Multivariate Cox Regression of recurrence
Read Also: Thyroid And Menopause Weight Gain
What Is Papillary Thyroid Cancer
Papillary thyroid cancer begins in the follicular cells in your thyroid that produce thyroglobulin . Its the most common type of thyroid cancer.
Your thyroid is a small, butterfly-shaped gland located at the front of your neck under your skin. Its a part of your endocrine system and controls many of your bodys important functions by producing and releasing certain hormones.
PTC tends to grow very slowly and usually develops in only one lobe of your thyroid gland.
There are several subtypes of papillary thyroid cancers. Of these, the follicular subtype is the most common. Other subtypes of papillary cancer arent as common and tend to grow and spread more quickly. They include:
Papillary thyroid cancer is also called papillary thyroid carcinoma.
Papillary Thyroid Cancer Quick Facts:
- Peak onset ages 30 through 50
- Females more common than males by 3 to 1 ratio
- Prognosis directly related to tumor size
- Accounts for 85% of thyroid cancers
- Can be caused by radiation or x-ray exposure
- Spread to lymph nodes of the neck present in up to 50% of cases
- Distant spread is very rare
- Overall cure rate very high
Also Check: Thyroid And Swollen Lymph Nodes
How Is Papillary Thyroid Cancer Diagnosed
Papillary thyroid cancer usually presents as a lump or nodule on your thyroid gland. You may notice it, or your healthcare provider may discover it during a routine neck examination. Sometimes, the nodule is discovered incidentally by imaging tests you get for other medical reasons.
Your healthcare provider will likely order the following tests to help diagnose PTC:
- Imaging tests: Your provider may order imaging tests to identify the nodule on your thyroid. These tests might include thyroid ultrasound, CT scan and/or magnetic resonance imaging .
- Fine needle aspiration : Your provider will likely want to take a small tissue sample, called a biopsy, from the nodule on your thyroid using a very thin needle. A pathologist will look at the tissue under a microscope to see if there are cancer cells and, if so, what type of thyroid cancer it is.
Your healthcare provider may also recommend genetic counseling to see if you have a genetic condition that may have caused PTC and may cause other types of tumors.
Prognostic Factors For Persistent Disease
Prognostic factors for persistent disease are shown in . Univariate analysis showed that older age, larger tumor size, higher number of metastatic LN, higher number of ECE-LNs, and central location of the metastatic LN were significantly associated with persistent disease. The numbers of LN metastases and ECE-LNs were closely linked. However, the number of ECE-LNs and tumor size were independent prognostic factors for persistent disease. When the tumor size was smaller than 4 cm with 10 or fewer metastatic LN or three or fewer ECE-LNs, the frequency of persistent disease ranged from 10 to 13% . Of note, patients with five or fewer metastatic LNs disclosed a frequency of persistent disease of 7%. When the tumor size was smaller than 4 cm with more than 10 metastatic LNs or more than three ECE-LNs or when tumor size was 4 cm or more without any of these LN criteria, the frequency of persistent disease ranged from 20 to 45%. In contrast, when the tumor size was 4 cm or more, with more than 10 metastatic LNs or more than three ECE-LNs, the frequency of persistent disease reached 75%. Interestingly, persistent disease was not found in any of the 26 patients without involvement of the central compartment, whereas it occurred in 27% of the 122 patients with central LN metastases.
Also Check: Hair Loss From Thyroid Disease
Papillary Thyroid Cancer Overview
Papillary thyroid cancer is the most common of all thyroid cancers . It can also be called papillary thyroid carcinoma since carcinoma implies a certain type of cancer. Since thyroid cancer is relatively common, and papillary thyroid cancer is the most common form of thyroid cancer, it is very likely that you will know somebody that had or has this form of cancer. Papillary thyroid cancer typically starts within the thyroid as growth, or bump on the thyroid that grows out of the otherwise normal thyroid tissue. Papillary thyroid cancer is clearly increasing in its incidence both in the United States and globally–it is one of the few cancers that are becoming more common, but we don’t know why this is happening. Our Introduction to Thyroid Cancer page has a great general overview of all types of thyroid cancer–read it if you haven’t already!
Recurrence Of Thyroid Cancer
Although thyroid cancer recurrence is not common, there are many treatment options available if it happens. If a cancer recurrence is detected in the neck lymph nodes, the best course of action is usually an operation to remove the affected node or additional treatment with RAI ablation. In order to determine the best treatment for recurrent thyroid cancer, it is critical to work with an experienced team of thyroid specialists.
Don’t Miss: What Happens If Thyroid Cancer Goes Untreated
Data Extraction And Quality Evaluation
Two authors abstracted the following data from the included articles: first author, countries of study, years of publication, study design, study population , number of cases, surgical intervention, and PTC-related risk factors. Age, gender, multifocal, tumor size, location, vascular invasion, thyroiditis , bilateral, and Hashimoto’s thyroiditis were the risk factors of LNM in PTC patients. The Newcastle-Ottawa quality assessment scale was used to assess the quality of the research .
What Are Some Other Papillary Thyroid Cancer Treatments

The other surgical option for patients with papillary thyroid cancer is a total thyroidectomy . An expert pre-operative evaluation of the papillary thyroid cancer patient is required to determine whether there is any involvement of the lymph nodes in the neck. In most circumstances, the involvement of neck lymph nodes can be determined prior to the thyroid surgery procedure. When there is evidence that the papillary thyroid cancer has spread to lymph nodes in the neck, surgical approaches to the central and lateral neck lymph nodes should be performed.
When neck lymph nodes are involved with papillary thyroid cancer, either during the evaluation of the papillary thyroid cancer or during surgery for the papillary thyroid cancer, the recommended operation is a total thyroidectomy.
Often, other characteristics of the tumor that can be seen under the microscope which may have an influence on whether the surgeon should remove the entire thyroid .
The surgical options are covered in greater detail in our article on for thyroid cancer. A more detailed discussion of thyroid surgery for the thyroid gland and lymph nodes of the neck can be found here.
Read Also: Environmental Causes Of Thyroid Disease
First Year Management After Initial Treatment
In patients treated with 131I and without suspected residual locoregional or distant disease , the usual procedure to ensure total thyroid ablation was to perform, at 612 months, a diagnostic WBS after 185MBq 131I, and to measure serum thyroglobulin and anti-Tg antibodies on thyroid-stimulating hormone stimulation. This procedure was done following withdrawal of thyroid hormone treatment or recombinant TSH . Total thyroid ablation was also confirmed by negative post-therapeutic WBS in patients treated with at least two therapeutic activities of 131I . No evaluation was done at 612 months for the other 19 patients.
How Is Papillary Thyroid Cancer Treated
Treatments for papillary thyroid cancer depend on the tumor size and whether the cancer has spread .
Surgery is the most common treatment for PTC. Depending on the tumors size and location, your surgeon may remove part of your thyroid gland or all of your gland . If you have cancer present in the lymph nodes of your neck, your surgeon may remove the affected lymph nodes at the time of the initial thyroid surgery or as a second procedure.
If you have a total thyroidectomy, youll need to take thyroid hormone replacement medication for the rest of your life.
Additional treatments for PTC include:
- Radioiodine therapy: Thyroid cells and papillary thyroid cancer cells absorb iodine, a mineral found in some food. Because of this, healthcare providers sometimes use a radioactive form of iodine to destroy all remaining normal thyroid tissue and potentially destroy residual cancerous thyroid tissue after a thyroidectomy.
- Radiation therapy: Radiation kills cancer cells and stops them from growing. External radiation therapy uses a machine to deliver strong beams of energy directly to the tumor site. Internal radiation therapy involves placing radioactive seeds in or around the tumor.
- Chemotherapy: Intravenous or oral chemotherapy drugs kill cancer cells and stop cancer growth. Very few people diagnosed with thyroid cancer will ever need chemotherapy.
Recommended Reading: Only Natural Pet Feline Thyroid Wellness
Risk Factors For Lymph Node Metastasis In Papillary Thyroid Carcinoma: A Systematic Review And Meta
- 1School of Public Health, The Key Laboratory of Environmental Pollution Monitoring and Disease Control, Ministry of Education, Guizhou Medical University, Guiyang, China
- 2College of Pharmaceutical Sciences, Southwest University, Chongqing, China
- 3College of Food Science, Guizhou Medical University, Guiyang, China
- 4Institute of Deep-Sea Science and Engineering, Chinese Academy of Science, Sanya, China
- 5Department of Endocrine and Breast Surgery, The First Affiliated Hospital of Chongqing Medical University, Chongqing, China
- 6Department of Pharmacology, College of Pharmacy, Guilin Medical University, Guilin, China
Purpose: To explore the risk factors that may predict the lymph node metastasis potential of these lesions and new prevention strategies in papillary thyroid carcinoma patients.
Materials and Methods: In total, 9,369 papillary thyroid carcinoma patients with 37.17% lymph node metastasis were analyzed in this study. The PubMed and Embase databases were used for searching works systematically that were published through to January 22, 2020.
The systematic review and meta-analysis defined several significant risk factors of lymph node metastasis in papillary thyroid cancer patients: age , gender , multifocality, tumor size , tumor location , capsular invasion, and extra thyroidal extension. Bilateral tumors and Hashimoto’s thyroiditis were unrelated to lymph node metastasis in patients with papillary thyroid cancer.
Value And Rationale For C
With the current practice of intense postoperative surveillance searching for even miniscule disease, the efforts to achieve thorough lymph node dissection are worth serious consideration. Because therapeutic lymph node dissection is virtually unanimously supported, the focus of debate has revolved around what is termed prophylactic dissectionremoving nodes even when not grossly abnormal in the judgment of the surgeon. Also, until recently, few in Western countries have supported lateral jugular lymph node dissection . Therefore, C-VI prophylactic node dissection has attracted considerable attention and investigation. The reasons to undertake routine C-VI lymph node dissection include:
- Preoperative US in the initial cervical exploration is nearly blind to the detection of LNM in C-VI
- Surgeons cannot reliably differentiate innocent from LNM in many cases
- LNMs occur in up to 50% of patients operated on for PTC
- Missed LNM are typically found along the recurrent laryngeal nerve in the trachea-esophageal groove, a potentially dangerous location if reoperation becomes necessary
- Dissection would logically lead to reductions in relapse and consequently reoperation
- C-VI dissection can be accomplished safely, although this is a major statement of contention
- Disease staging could be changed for patients over 45 years, from stage I to stage III, with potential for additional treatment implications
- RAI is unreliably effective in cleaning up residual macroscopic LNM.
Read Also: For Thyroid Test Is Fasting Needed
What Is The Prognosis Of Papillary Thyroid Cancer
Overall, the prognosis of papillary thyroid cancer is excellent, especially if youre younger than 40 at diagnosis and have a small tumor. PTC can often be treated successfully and is rarely fatal, even if it has spread to lymph nodes in your neck.
Factors that may lead to a worse prognosis include:
- Being older than 55 years at diagnosis.
- Having a large tumor.
- If the cancer has spread to distant parts of your body.
- If you have a rare subtype of PTC, which are typically more aggressive, including the tall cell variant, diffuse sclerosis variant or solid variant.
After Surgery: Radioactive Iodine And Long
Almost all people who had surgery for papillary thyroid cancer will need to see a doctor for many years to have exams and certain blood tests to make sure the cancer has been cured, and to detect any return of the cancer as soon as possible should it return. Many people with papillary thyroid cancer will need to take radioactive iodine to help cure the cancer. We have several very important pages on these topics.
Read Also: Over The Counter Thyroid Booster
Recurrence Of Ptc After Optimized Surgery
Having considered in detail the disease PTC, aspects of optimized surgery for this disease, and different forms and implications of disease recurrence, a coherent management plan can be synthesized.
As evidence in support of this approach, the results are presented of the Mayo Clinic moderate surgical approach including preoperative US for detection and mapping of LNM NTTx or TTx routine C-VI CLND, and lateral internal jugular lymph node dissection when indicated by either positive nodes detected by palpation or US. From 1999-2006, 420 patients were treated with this comprehensive approach, and excluded only the few patients who were found intraoperatively to be unresectable. Tumors were multicentric in 40%, averaged 1.7 cm in size, were bilateral in 30%, demonstrated extrathyroidal extension in 17%, were associated with C-VI LNM in 51% and lateral LNMs in 20%, and had MACIS low-risk prognostic scores in 84%. RAI was used in 40% of patients. Relapse of LNM occurred in previously operated fields in 5% of patients 3% had true local recurrence or distant metastasis, with complications limited to 1.2% hypoparathyroidism and only a single patient suffered unintentional RLN paralysis. Only a single patient had died as a direct result of PTC at last follow-up.