Characteristics Of Pdtc Cases Stratified By Tg Group
Patients with undetectable and detectable Tg levels showed no significant age or gender differences . Around two-thirds of all cases were older than 45 years and the female-to-male ratio was also similar in both groups .
Table 1.
Characteristics stratified by Tg group
Pathological tumor characteristics in the 2 groups were only statistically different for surgical margins and nodal status patients with detectable Tg had a lower probability of achieving R0 margins and a higher node status . Nevertheless, these patients showed a trend towards more advanced local disease with a higher pT4 status and more frequent extrathyroid extension . No statistical significant differences between the 2 groups were found regarding the size of primary tumor, vascular invasion, or histological subtype.
Poorly Differentiated Thyroid Cancer Support
| Meets: | The ThyCa Poorly Differentiated Support Group holds free virtual meetings on the second Saturday of each month at Noon to 1:30 pm Eastern Time. This group discusses topics of interest regarding people who have been diagnosed with poorly differentiated thyroid cancer. Poorly differentiated thyroid cancer is an aggressive form of follicular cell derived thyroid cancer with a prognosis intermediate between the often slow growing papillary or follicular thyroid cancers and the rapidly growing often fatal anaplastic thyroid cancer. Note: Not all papillary or follicular cancers are slow growing.Please email our group facilitator at for answers to any questions and the instructions on how to join us. Once we give you the instructions, they will be good for all our meetings. |
| Location: | |
| Please check your spam folder for an email if you don’t hear from us. | |
| Other Notes: | On Friday, Saturday, and Sunday, October 22-24, 2021, you are cordially invited to the 24th International Thyroid Cancer Survivors’ Virtual Conference. This free event is sponsored by ThyCa: Thyroid Cancer Survivors’ Association, Inc. |
Visit to register for the conference and for additional information as it becomes available.
Patient Tumor And Treatment Characteristics
Of the 91 patients, 62% were female. Median age was 59 years . Sixteen patients had a history of head and neck radiation exposure.
Fifty patients had a primary tumor of 4 cm or less. Primary tumor staging included four pathological T stage 1 patients, 14 pT2, 46 pT3, and 27 pT4a. Twenty-two patients had pathological N stage 0 neck, 14 pN1a, and 22 pN1b, and one patient had no recorded location . Thirty-two patients had clinically negative neck without any neck dissection . Twenty-four patients presented with distant disease, and an additional 14 developed distant disease . One patient developed bone metastasis after clearance of lung disease on computed tomography scans after RAI therapy.
Of all 91 PDTC patients, five had gross residual disease postoperatively, and an additional 45 had microscopic positive margins. At initial surgery, 18 patients had central neck dissection alone, 23 had central plus lateral neck dissection, whereas 18 patients had only intraoperative lymph node sampling for a small number of indeterminate central compartment nodes.
Out of 24 patients with distant disease at presentation , 17 had RAI-avid M1 disease, four had non-RAI-avid M1 disease, two did not undergo RAI treatment, and no data were available for one patient . Six patients had PET-positive M1 disease, nine had PET-negative M1 disease, and no PET scans were done in nine patients with M1 .
Also Check: What Thyroid Tests Should I Ask For
Molecular Characteristics Of Pdtc In Light Of Next
In an effort to elucidate the molecular characteristics of PDTC that are responsible for driving disease progression, several groups have published genomic findings in PDTC using next-generation sequencing techniques . The study by Landa et al. using the MSK-IMPACT NGS platform has been the largest and the most comprehensive published study on PDTC to date. It examined the largest PDTC cohort , with targeted sequencing of all exons and selected introns of 341 cancer-related genes. Studies by Gerber et al. , Nikiforova et al. , and Sykorova et al. also examined relatively smaller numbers of PDTC patients with sequencing of select exons and hotspot regions of cancer-related genes .
Hurthle Cell Thyroid Cancer
Hurthle cell thyroid cancer is a rare sub-type of follicular thyroid cancer. Approximately 3% of thyroid cancer cases are Hurthle cell. Hurthle thyroid cells can be benign or cancerous. Benign Hurthle cells usually do not recur once they are removed.
Hurthle cells are larger than follicular cells and have a pink-staining quality. Hurthle cell thyroid cancer tends to affect older adults and has a slightly poorer prognosis than follicular and papillary types. It spreads to the lymph nodes about 20% of the time.
Read Also: Location Of The Thyroid Gland
Targeted Therapies Against Mapk Pathway
Mitogen-Activated Protein Kinase pathways connect extracellular signals to the network that controls cell proliferation, motility, and cell death. Thyroid cancer often presents genetic alterations that activate the MAPK pathway. These mutations include point mutations in BRAF and RAS or RET/PTC translocations . These mutations have been widely studied as a new therapeutic target in advanced thyroid cancer.
Vemurafenib and dabrafenib are BRAFV600E inhibitors that function as ATP-competitive inhibitors. Vemurafenib has a much higher selectivity for mutated BRAF compared to wild type BRAF . A multicenter, phase I study of vemurafenib, included three patients with BRAFV600E mutated RAI-refractory-metastatic thyroid cancer , treated with different doses of vemurafenib at 240360 mg twice daily, and later increased to 720 mg twice a day. One patient had a partial response with a 31% reduction of the target lesion in the lungs, and the other two patients had stable disease . The progression-free interval for the three patients were 11.4, 11.7, and 13.2 months, and the overall survival was 15, 21, and at least 31.7 months. The adverse events were similar to those were reported in a phase I study of patients with metastatic melanoma.
Clinical Features And Pathogenesis
Poorly differentiated thyroid carcinomas include a heterogeneous group of neoplasms whose behavioral and histologic features are intermediate between well-differentiated and undifferentiated thyroid carcinomas.267269 The best described tumor of this group is classified as insular carcinoma. The frequency of this tumor type appears to differ in different geographic regions. In central Italy, the tumors account for approxi mately 4% of all thyroid carcinomas. It is much less common in the United States and most other countries.
There is a slight female predominance, and the median age at diagnosis is 55 years. Most patients present with a thyroid mass of variable duration. Analysis of several series of cases revealed regional metastases in 36% and distant metastases in 26% at presentation.219
Zubair W. Baloch, Virginia A. LiVolsi, in, 2021
Don’t Miss: For Thyroid Test Is Fasting Needed
General Information About Thyroid Cancer
In This Section
Thyroid cancer includes the following four main types:
For clinical management ofthe patient, thyroid cancer is generally divided into the following two categories:
Well-differentiated tumors are highly treatable and usually curable. Poorly differentiated and undifferentiated thyroid tumors are less common, aggressive, metastasize early, and have a poorer prognosis. Medullary thyroid cancer is a neuroendocrine cancer that has an intermediate prognosis.
Thethyroid gland may occasionally be the site of other primary tumors, includingsarcomas, lymphomas, epidermoid carcinomas, and teratomas. The thyroid may also be the siteof metastasis from other cancers, particularly of the lung, breast, and kidney.
Rai And Histological Phenotype In Patients With Detectable And Undetectable Tg
The study included 38 cases from 1986 to 2011 .
After total thyroidectomy and RAI, 15 patients had detectable and 23 had undetectable Tg levels. Patients received a median cumulative activity of 8.362 GBq . Patients with detectable Tg and undetectable Tg levels received a median cumulative activity of RAI of 8.362 GBq and 6.771 GBq, respectively . Only 1 patient received an activity < 3.7 GBq.
The pathological subtypes in the 15 patients with detectable Tg were insular , solid , trabecular , and mixed phenotype . In the 23 patients with undetectable Tg, these were insular , solid , trabecular , and mixed phenotype .
Don’t Miss: Braf Mutation Papillary Thyroid Cancer
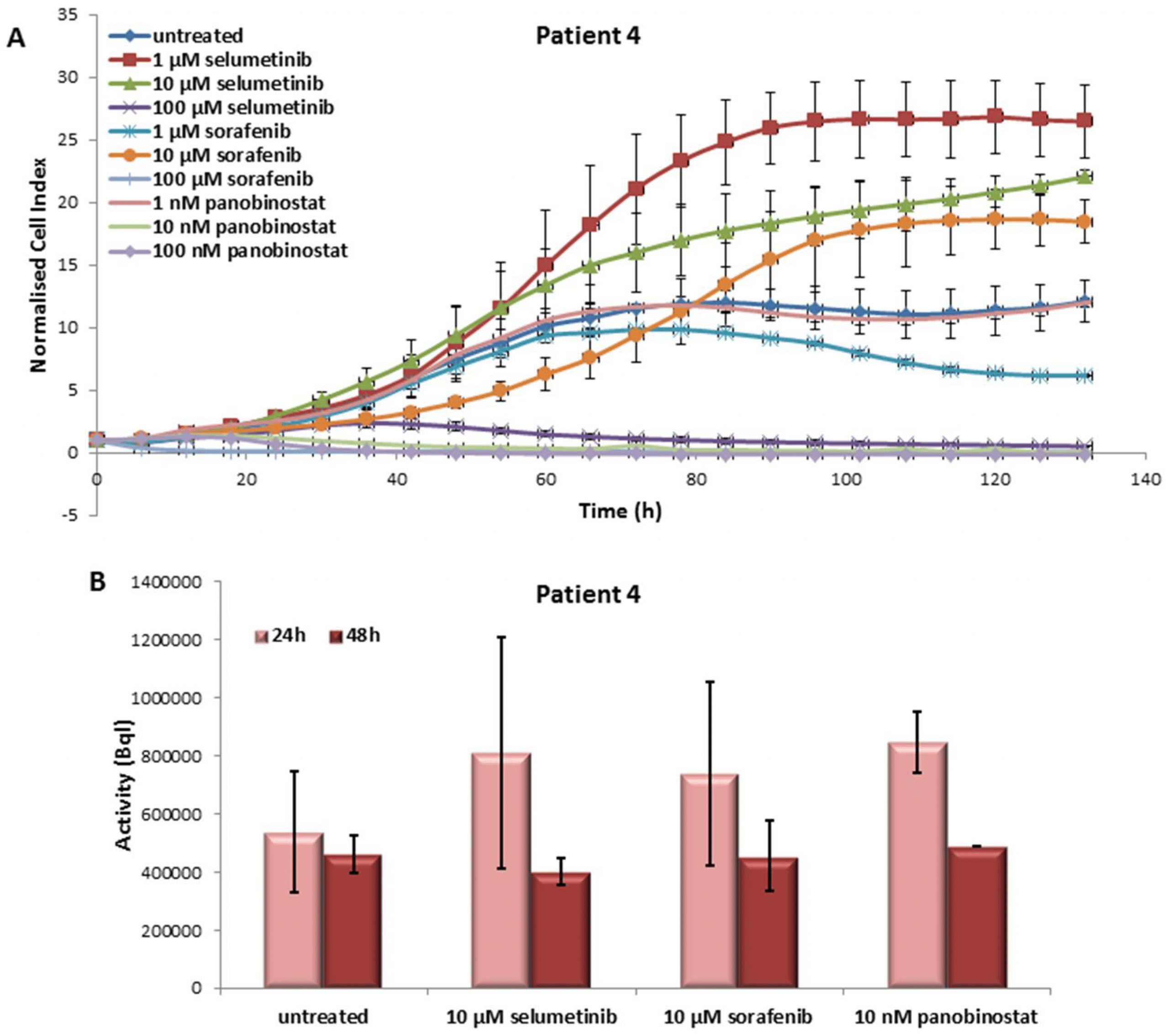
In Vitro Results Of The Fifth Patient
The fifth patient was affected by PDTC and the overall survival was 174 weeks after his first diagnosis. The patient received once radiotherapy. Afterwards, the patient was treated with sorafenib and then with lenvatinib. Both treatments were interrupted because of severe adverse events. RAI-R was diagnosed. No mutation of BRAF was detected . The treatment with TKIs and panobinostat was applied at the cells derived from his resected tumor after they have been kept proliferating in in vitro culture conditions.
3.5.1. Effects on Cell Viability of the Individual Tumor Cells Caused by Treatment with Sorafenib, Panobinostat and Selumetinib
In the PDTT cells of the fifth patient case, selumetinib caused a reduction of cell viability at 100 µM only. Treatment with sorafenib was able to reduce significantly the cell viability at 1 µM already. In addition, 10 and 100 nM panobinostat showed, once again, the strongest efficacy in cell viability reduction .
Effects of selumetinib, sorafenib and panobinostat on cell viability and RAI-U. Real time cell viability of PDTT cells treated with 1 to 100 µM selumetinib and sorafenib and 1 to 100 nM panobinostat . RAI-U after 24 and 48 h of treatment with 10 µM selumetinib, 10 µM sorafenib and 10 nM panobinostat . Shown are means of experiments performed in triplicates ± SD /SEM .
3.5.2. Radioiodine Up-Take after Treatment with Sorafenib, Panobinostat and Selumetinib
3.5.3. Expression of SLC5A5 , HMGA2 and miRNAs
Patient And Tumor Factors Predictive Of Dss
Age 45 years, pT size 4 cm, higher pT, ETE, positive margins, and distant metastasis at presentation were predictive of worse outcome on univariate analysis . Multivariate analysis of age, pT stage, and M1 showed that pT4a stage and M1 remained independent predictors of worse DSS. Patients with pT4a disease were seven times more likely to die of disease compared to those with pT1/2 disease . Patients with M1 disease were three times more likely to die of disease compared to those without M1 disease . pT size and ETE were not used in the multivariate analysis because they were incorporated in the pT stage variable.
A, Five-year DSS stratified by pathological T stage. B, Five-year DSS stratified by M status.
Don’t Miss: If Thyroid Levels Are High
Targeting Of Pi3k/akt Pathway
The PI3K/Akt pathway plays a crucial role in thyroid carcinogenesis, cell dedifferentiation, invasion, and metastasis. The three main players of these pathways are PI3K, Akt, and mTOR. Activating mutations and copy gain in the gene coding for the catalytic subunit of PI3K , and inactivating mutations and hypermethylation of the tumor suppressor gene PTEN have been identified in advanced DTC especially follicular thyroid cancer and ATC. These genetic and epigenetic alterations result in angiogenesis, drug resistance, and thyroid cancer progression and metastasis. The targeting of the PI3K/Akt/mTOR has been an active area of cancer research. Several inhibitors showed promising anti-tumor activity in thyroid cancer cells in vitro and in vivo.
In another phase II clinical trial assessing the efficacy of everolimus in a cohort of patients with advanced thyroid cancer, everolimus was administered at the dose of 10 mg daily. Sixty-five percent of patients with differentiated thyroid cancer showed a stable disease as the best response. Forty-six percent of the patients required a dose reduction because of the toxicity of everolimus. Analysis of the somatic mutations in patients’ samples did not show any association between mutation status and response to everolimus .
How Much Poorly Differentiated Is Needed
It has long been known that there are PDTCs with a minor and even a major component of a well-differentiated thyroid carcinoma like PTC or FTC. Today, it is believed that most of them arise in a well-differentiated thyroid carcinoma, although a subset of these lesions apparently also arise de novo . About 80% of PDTC have a PD component of > 50%, and only 20% of PDTC have a minor PD component . However, it was unclear in the Turin proposal what percentage of poorly differentiated was needed in a tumor to allow for such a diagnosis andmore importantlyto affect patient prognosis moreover, the 2004 WHO classification did not offer a cut-off value . We showed that even a small PD component of 10% affects patient prognosis equally negative as a tumor that consists of 100% PD regarding relapse-free survival or overall survival . Our findings were recently confirmed by others and are now reflected in the current WHO classification . Therefore, a thorough histological work-up is highly recommended to ensure an adequate diagnosis is made.
Stepwise de-differentiation of thyroid carcinomas derived from follicular epithelial cell
Recommended Reading: What Can I Do To Help My Underactive Thyroid
Cellular Classification Of Thyroid Cancer
In thyroid cancer, cell type is an important determinant of prognosis and treatment. The thyroid has two cell types: follicular cells and parafollicular C cells. The management of thyroid cancer depends on the cell of origin and how well the integrity of the cell type is maintained. The four main types of thyroid cancer are divided into the following two categories for clinical management:
Differentiated thyroid cancers.
Parafollicular C cell thyroid cancers.
Other types .
References
Standard Treatment Options For Papillary And Follicular Thyroid Cancer
Localized/regional papillary and follicular thyroid cancer
Surgery is the therapy of choice for all primary lesions. Surgical optionsinclude total thyroidectomy or lobectomy. The choice of procedure isinfluenced mainly by the age of the patient and the size of the nodule. Survival results with the two procedures are similar for early-stage disease, with differences in the ratesof surgical complications and local recurrences.
Standard treatment options for localized/regional papillary and follicular thyroid cancer
Standard treatment options for localized/regional papillary and follicular thyroid cancer include the following:
Surgery
The objective of surgery is to completely remove the primary tumor, while minimizing treatment-related morbidity, and to guide postoperative treatment with RAI. The goal of RAI is to ablate the remnant thyroid tissue to improve the specificity of thyroglobulin assays, which allows the detection of persistent disease by follow-up whole-body scanning. For patients undergoing RAI, removal of all normal thyroid tissue is an important surgical objective. Additionally, for accurate long-term surveillance, RAI whole-body scanning and measurement of serum thyroglobulin are affected by residual, normal thyroid tissue, and in these situations, near total or total thyroidectomy is required. This approach facilitates follow-up thyroid scanning.
Total thyroidectomy
Evidence :
Lobectomy
Radioactive iodine therapy
Evidence :
Read Also: What Percentage Of Thyroid Biopsies Are Cancerous
Follicular Cell Thyroid Cancers
From well differentiated to undifferentiated, the types of thyroid cancer from follicular cells are:
Papillary thyroid cancer: This is typically the least aggressive type of thyroid cancer. It accounts for about 80% of thyroid cancer diagnoses. While papillary thyroid cancer usually occurs in only one lobe of the thyroid gland, it appears in both lobes in 10%-20% of cases. Papillary thyroid cancer is most common in women of childbearing age. Its treatment is successful in most patients.
Follicular thyroid cancer: This accounts for about 10% of thyroid cancers. Though it can be more aggressive than papillary thyroid cancer, follicular thyroid cancer usually grows slowly. Treatment for follicular thyroid cancer is similar to papillary thyroid cancer and is successful for most patients.
Both papillary and follicular thyroid cancer are considered well differentiated cancers. Well differentiated thyroid cancer tends to stay contained within the thyroid gland. When it does spread outside the thyroid, the most common locations of spread, or metastasis, are lymph nodes, lungs, bones and the liver.
Hürthle cell thyroid cancer: Also called oxyphilic cell carcinoma, Hürthle cell carcinoma was considered a type of follicular thyroid cancer until recently. Most patients diagnosed with Hürthle cell carcinoma do well, but the outlook may change based on the extent of disease at the time of diagnosis.
Patients And Pretreatment Evaluations
This study was approved by our institutions ethics committee . Between February 2011 and April 2012, we analyzed the outcomes of 5 unresectable PDTC patients treated with IMRT in our institution. There were 2 males and 3 females with a median age of 55 years . All patients had histologically confirmed PDTC. Patient 4 and 5 had evidence of lung metastases before the start of treatment, and patient 3 presented with recurrent disease. The clinical characteristics of the five patients are listed in Table 3. The initial evaluation of the patients included medical history and physical examination, routine labs, computed tomography scans of the chest and neck, abdominal ultrasound, and bone scintigram. Additional investigations were performed only on those patients with suspicious findings. All patients in this study had advanced unresectable disease. The patients disease was staged according to the seventh AJCC Cancer Staging Manual as follows: 3 were T4bN1bM0, and 2 were T4bN1bM1 .
Table 3: Patients characteristics
Abbreviations: M, male F, female.
Also Check: How To Test For Overactive Thyroid
In Vitro Results Of The Second Patient
The second patient was affected by ATC and survived for eight weeks after the first diagnosis. He received palliative treatment only and was characterized by RAI-R. No mutation of BRAF was detected . He received palliative treatment and no individualized therapy was established. The treatment with TKIs and panobinostat was applied at the cells derived from his resected tumor after they have been kept proliferating in in vitro culture conditions.
3.2.1. Effects on Cell Viability of the Individual Tumor Cells Caused by Treatment with Sorafenib, Panobinostat and Selumetinib
The PDTT obtained from the tissue of this patient showed a significant reduction of cell viability with 100 µM selumetinib and sorafenib . Panobinostat showed a significant effect at 10 and 100 nM that determined a reduction of the growth curve to zero values.
Effects of selumetinib, sorafenib and panobinostat on cell viability and RAI-U. Real time cell viability of PDTT cells treated with 1 to 100 µM selumetinib and sorafenib and 1 to 100 nM panobinostat . RAI-U after 24 and 48 h of treatment with 10 µM selumetinib, 10 µM sorafenib and 10 nM panobinostat . Shown are means of experiments performed in triplicates ± SD /SEM .
3.2.2. Radioiodine Up-Take after Treatment with Sorafenib, Panobinostat and Selumetinib
3.2.3. Expression of SLC5A5 , HMGA2 and Their Regulatory miRNAs
3.2.4. Expression of NIS Protein Level