Papillary And Follicular Thyroid Cancer Stage Iv
If you are at stage IV, it means the cancer has spread. Your doctor assigns the letters âA,â âBâ and âCâ to show how far.
- Stage IVA — The cancer has spread beyond your thyroid. It now is under your skin, or it affects your larynx, esophagus or trachea. A smaller tumor in more distant lymph nodes is also considered stage IVA.
- Stage IVB — The tumor has grown toward your spine or into nearby large blood vessels, like the carotid arteries. These carry blood to your brain, face, and neck. It might have also spread to your lymph nodes.
- Stage IVC — The cancer has spread beyond the thyroid, and to distant sites of the body. It may be in your lungs, bones, and lymph nodes.
Survival Rates By Tnm Stage
The first approach is based on the TNM stage. Statistical survival times are matched to the stage of the disease.
| TNM Lung Cancer Stage | |
|---|---|
| M1c | 6.3 months |
By contrast, the one-year survival rate for stage 4 lung cancer was reported in one study to be between 15% and 19%. This means this portion of patients with metastatic disease lived for at least a year.
Subgroup Analysis According To The Histologic Type Of Thyroid Cancer
There were 106 DTC patients and 28 of them died of the disease. Asymptomatic screening and symptomatic group did not show a statistically significant difference in disease specific death before 2004. However, asymptomatic group showed a significantly improved prognosis only after 2004 For PDTC, MTC and ATC, survival analysis could not performed because of the small number of patients in each subgroup .
Also Check: Does Selenium Help Thyroid Eye Disease
Multivariable Cox Proportional Hazards Model
Predictors of 5-year DSS included advanced disease and larger tumor size . There was no association between 5-year DSS and gender, number of co-morbidities, race, type of surgery performed, insurance coverage, or hospital volume. The administration of radioactive iodine was protective . The hazard ratio for death from PTC at 5 years was 38 times higher in patients 60 years, compared to patients < 45 years of age . Harrells c-statistic was 0.9452.
Table 2 Multivariable Cox-proportional hazards analysis of predictors of 5-year disease-specific survival
Predictors of 10-year DSS included advanced disease and larger tumor size . There was no association between 10-year DSS and hospital volume, race, co-morbidities, insurance, surgery performed, or gender. The administrative of RAI was protective, with hazard ratio of 0.60. The hazard ratio for death from PTC at 10 years after diagnosis was nearly 30 times higher in patients 60 years, compared to patients < 45 years of age . Harrells c-statistic was 0.9328.
Table 3 Multivariable Cox-proportional hazards analysis of predictors of 10- year disease-specific survivalTable 4 Multivariable Cox-proportional hazards analysis of predictors of 5- year disease-free survivalTable 5 Multivariable Cox-proportional hazards analysis of predictors of 10- year disease-free survival
Brain Metastases From Differentiated Thyroid Carcinoma: A Retrospective Study Of 22 Patients
- Department of Head and Neck Surgery, Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center of Cancer Medicine, Guangzhou, China
Background: Brain metastasis from differentiated thyroid cancer has followed a similar increasing trend to that of thyroid cancer in recent years. However, the characteristics and treatments for brain metastases are unclear. The aim of this study was to understand this disease by analyzing patients with brain metastases from differentiated thyroid cancer .
Methods: Between 2000 and 2020, the database of the Sun Yat-sen University Cancer Center was searched for differentiated thyroid cancer patients. We identified a cohort of 22 patients with brain metastases. The characteristics of the patients, histological features, treatments, and time of death were reviewed. The overall survival rate was calculated using the Kaplan Meier method. Survival curves of different subgroups were compared according to baseline characteristics and treatments received.
Brain metastasis from differentiated thyroid cancer has a poor prognosis. However, it can be improved by comprehensive treatment. PS of the patients can greatly affect survival. Skull metastases have improved prognosis over intracranial types. Radioiodine therapy appears to effectively improve the prognosis of patients with skull metastases from DTC.
Also Check: Most Common Form Of Thyroid Cancer
What Is The Thyroid Cancer Survival Rate
For people with differentiated thyroid cancer , age is the most important prognostic factor. If a patient is younger than 45, they are considered a Stage II and have an excellent prognosis .
For people with medullary thyroid cancer, age is not as important a predictor of outcome. In general, those with medullary thyroid cancer that has not spread beyond the thyroid , have a 95% 10-year survival. Patients with medullary thyroid cancer that has spread to the neck lymph nodes have a 10-year survival of 75%. For those patients with metastatic medullary thyroid cancer, the 10-year survival is 20 to 40%
For people with anaplastic thyroid cancer, the 5-year relative survival rate is around 5%.
Side Effects Of Thyroid Hormone Treatment
Thyroid hormone pills themselves do not usually cause side effects, but it can take some time to get the dosage right, and you may experience symptoms of either or while you and your doctor work to determine the correct dose.
Symptoms of too much thyroid hormone may include:
-
Increased heart rate
Symptoms of too little thyroid hormone may include:
-
dry skin and hair
Definitely check in with your doctor if you feel you are experiencing any of the above symptoms so that your dosage can be properly adjusted.
You May Like: Best Thyroid Diet To Lose Weight
Where Do These Numbers Come From
The American Cancer Society relies on information from the SEER* database, maintained by the National Cancer Institute , to provide survival statistics for different types of cancer.
The SEER database tracks 5-year relative survival rates for thyroid cancer in the United States, based on how far the cancer has spread. The SEER database, however, does not group cancers by AJCC TNM stages . Instead, it groups cancers into localized, regional, and distant stages:
- Localized: There is no sign the cancer has spread outside of the thyroid.
- Regional: The cancer has spread outside of the thyroid to nearby structures.
- Distant: The cancer has spread to distant parts of the body, such as the bones.
Life After Thyroid Cancer Surgery #3 Follow Up Lab Tests And Scans
The Clayman Thyroid Center believes that thyroid cancer patient follow-up is best managed by an endocrinologist with defined expertise in the evaluation, management, and follow-up of thyroid cancer patients. Communication between the endocrinologist, surgeon, radiologist, and other members of the thyroid cancer team is critical. This is the absolute foundation of thyroid cancer treatment at the Clayman Thyroid Center.
After thyroid cancer surgery, your thyroid hormone levels should be checked in 4-6 weeks to see if thyroid hormone medication is needed or if your dose should be adjusted. You should have a complete history and physical exam along with an expert ultrasound done 6 months after thyroid cancer surgery and yearly after that. The following blood tests are always done routinely for surveillance and monitoring:
1) Free T4 level: This is the blood level of the major hormone normally produced by the thyroid gland. This is also a direct measurement of the most commonly prescribed thyroid hormone pill, levothyroxine or Synthroid. The dose of thyroid hormone pill will be based upon the blood thyroid stimulating hormone level described below.
Additional blood tests that are used to monitor medullary thyroid cancer are calcitonin and CEA .
A PET/CT scan in a patient with thyroid cancer spread to the lungs is seen below.
Check out this post for more information regarding staging and imaging for thyroid cancer along with follow-up.
You May Like: Can Thyroid Issues Cause Erectile Dysfunction
How Is Papillary Thyroid Cancer Staged
Papillary thyroid cancer staging is based on the results of the physical examination, biopsy, imaging tests and the pathologic findings of surgery itself .
Papillary thyroid cancer has a staging system that is not like other cancers. This staging system for papillary thyroid cancer takes into account the age of the patient. The break point of age in the American Joint Committee on Cancer staging system for papillary thyroid cancer is 55 years of age. Therefore, if you are less than 55 years of age, the most advanced papillary thyroid cancer is stage II disease.
In papillary thyroid cancer staging, and for that matter all cancer staging, the earlier the stage of disease is the more favorable and curable the cancer. Therefore, the lower/smaller the number, the better the chance for cure and long term survival. :1167-214.)
Pathological Analysis And Staging
Surgical specimens were analyzed and classified as papillary thyroid carcinoma or follicular thyroid carcinoma according to World Health Organization standard at the time of initial treatment. The present study used the histological classification given in the original pathology report. Considering that multiple revisions of the WHO standards took place over the course of the study and samples were analyzed by many different pathologists, we only classified patients as having papillary, follicular, or Hürthle cell DTC.
The primary tumor diameter was determined based on macroscopic analysis of the surgical specimen, when possible. This also was true for invasive carcinoma, with the pathologist making a best estimate in widely invasive cases. For multifocal tumors or in patients with both a papillary and a follicular carcinoma, the diameter of the largest tumor focus was taken for the primary tumor diameter. In cases of an unclear classification at the time of initial diagnosis, specimens were sent to the reference pathologist on thyroid histology for Germany.
Histological grading was not determined or reported because this is not recommended by the WHO. For the present study, we only included those tumors that were classified as papillary or follicular thyroid cancers, without including those classified as poorly differentiated or insular thyroid carcinomas.
You May Like: Can Thyroid Cancer Cause Pain In Back Of Neck
How Is Anaplastic Thyroid Cancer Diagnosed
Anaplastic thyroid cancer can present in several ways. Most often it presents as a lump or nodule in the neck. These tumors grow very quickly and often growth can be visible to the patient or the family and friends of the patient. In some cases, anaplastic thyroid cancer presents as a neck mass with difficulty swallowing, difficulty breathing, or hoarseness if one of the vocal chords is paralyzed by the tumor.
Typically, a fine needle aspiration or core biopsy is performed. Once the diagnosis is confirmed, a full assessment of the patients overall health should be completed. This includes blood tests, as well as imaging scans to determine if and where the cancer has spread.
All patients with Anaplastic Thyroid Cancer are diagnosed as Stage IV due to the aggressive nature of this tumor. There are three sub-stages:
- Stage IVA: Anaplastic thyroid cancer is present only in the thyroid
- Stage IVB: Anaplastic thyroid cancer is present in the thyroid and in the neck, but not in other parts of the body
- Stage IVC: Anaplastic thyroid cancer is present in the thyroid as well as other parts of the body, such as the bones, lungs or brain
About 10% of patients have anaplastic thyroid cancer that is present only in the thyroid, and approximately 40% of those diagnosed have cancer that is localized in the neck and/or lymph nodes. The remaining patients have anaplastic thyroid cancer that has metastasized to other parts of the body at the time of diagnosis.
Patient Characteristics And Histology
The basic conditions of the patients are shown in Table 2. Of the 22 patients, 12 were male and 10 female . The mean patient age was 54.5 years at BM diagnosis. Fourteen patients presented other previous and/or synchronous distant metastases: lung , bone , liver , skin . The mean interval time between diagnosis of the first metastasis and BM was 2 years for these patients.
Table 2 Individual clinical findings of patients with BRAIN metastases from DTC.
Fourteen patients had papillary carcinoma, six patients had follicular carcinoma and two patients were unknown. Stages were pT0-2 for 12 patients, pT3-4 stage for eight patients, and unknown for two patients. Nodal involvement was present for 17 patients, absent for three patients, and unknown for two patients. Twelve patients had histological confirmation that the brain lesions were of thyroid origin through biopsy or resection. Nine cases showed vascular invasion, while 10 cases showed no invasion. Three cases were unknown. Necrosis was absent in all cases. Moderate nuclear atypia was observed in 6 cases, where as in 14 cases it was severe. BRAF mutation was found in 9 cases, while 7 cases were not. Six cases were unknown. Seven of 9 cases with BRAF mutation showed vascular invasion, which occurred in only 2 of 7 cases of patients without BRAF mutation.
You May Like: How Long For Thyroid Medicine To Work
Death From Other Causes
Thirty-eight patients died from causes other than thyroid cancer. Two died from another pre-existing primary tumour and nine from a cardiac cause. The two patients who died from another pre-existing primary tumour suffered from chronic lymphatic leukaemia and acromegaly respectively and belonged to a group of 26 patients with a history of a primary tumour diagnosed before thyroid carcinoma. Ten of these 38 patients had evidence of persistent thyroid cancer at their latest visit.
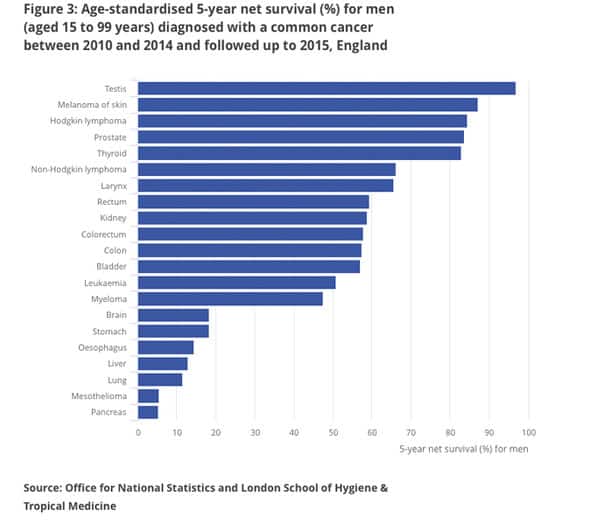
Thyroid Cancer Survival Rates By Type And Stage
Survival rates can give you an idea of what percentage of people with the same type and stage of cancer are still alive a certain amount of time after they were diagnosed. They can’t tell you how long you will live, but they may help give you a better understanding of how likely it is that your treatment will be successful.
Keep in mind that survival rates are estimates and are often based on previous outcomes of large numbers of people who had a specific cancer, but they cant predict what will happen in any particular persons case. These statistics can be confusing and may lead you to have more questions. Your doctor is familiar with yoursituation ask how these numbers may apply to you.
Recommended Reading: How To Feel Your Thyroid
How Is Thyroid Cancer Diagnosed
If you have an enlarged thyroid nodule or other signs of thyroid cancer, your healthcare provider may order one or more of these tests:
- Blood tests: A thyroid blood test checks hormone levels and gauges whether your thyroid is functioning properly.
- Biopsy: During a fine-needle aspiration biopsy, your healthcare provider removes cells from your thyroid to test for cancer cells. A sentinel node biopsy can determine if cancer cells have spread to lymph nodes. Your provider may use ultrasound technology to guide these biopsy procedures.
- Radioiodine scan: This test can detect thyroid cancer and determine if cancer has spread. You swallow a pill containing a safe amount of radioactive iodine . Over a few hours, your thyroid gland absorbs the iodine. Your healthcare provider uses a special device to measure the amount of radiation in the gland. Areas with less radioactivity need more testing to confirm the presence of cancer.
- Imaging scans:Radioactive iodine scan, computed tomography and positron emission tomography scans can detect thyroid cancer and cancer spread.
Dog Breeds Predisposed To Thyroid Cancer
Golden retrievers are at increased risk of developing two types of canine thyroid cancer: anaplastic thyroid cancer and lymphocytic thyroid cancer. Anaplastic thyroid cancer is rare and very aggressive.
Generally speaking, thyroid cancer tends to affect medium to large breed dogs.
Although thyroid cancer can occur in any dog, the following breeds appear more susceptible:
- Bernese Mountain Dogs
- Mixed-Breed Dogs
Read Also: How To Help Someone With Thyroid Problems
Clinical Features Of Bm
The mean number of BM was 2.3 . Eleven patients had a single BM while the remainders had multiple BMs. For 15 patients, BMs were revealed by neurologic symptoms, including headaches, nausea, motor or sensory deficits, ataxia, aphasia, confusion, and epileptic seizures. For the remaining seven patients, BMs were diagnosed by chance and presented no symptoms. Diagnoses were made by systematic cerebral imaging before TKI prescription for three patients, by iodine scans for four patients, by PET/CT scans for two patients, by magnetic resonance imaging for three patients, and by enhanced computed tomography for three patients. WHO PS at BM diagnosis was good for 14 patients and poor for eight. For 16 patients, CT images or MRI were available and reviewed. Five patients had metastatic tumors where the main tumor was located in the skull the remaining 17 cases were located intracranially.
Side Effects Of Thyroid Surgery
The risks of thyroid surgery include:
-
Damage to the laryngeal nerve. It can be stunned, or one vocal cord wont move the same way as the other, Dr. Harari explains. About 5% of people temporarily experience this complication, and 1% have permanent damage. There are procedures to regain vocal strength, and an ENT specialist can assist the patient in these efforts.
-
Hypoparathyroidism, or, as sometimes surgeons decide to remove one or more of the parathyroid glands four tiny glands that regulate the bodys calcium levels and are located near the back of the thyroid. People whose thyroid surgery involves a central neck incision have a 10% risk of parathyroid complications.
-
Vagus nerve issues. Lateral neck incisions can risk impacting the vagus nerve, Dr. Harari says. This can have effects on the voice as well as the shoulder or tongue.
-
Loss of thyroid function. After surgery, you will probably need to take pills for the rest of your life to replace lost thyroid hormones. If your parathyroid glands are also removed, you may also need to take calcium and vitamin D.
Don’t Miss: What Type Of Doctor Treats Thyroid Conditions