New Uchicago Medicine Research Sheds Light On Outcomes As Cases Increase Dramatically
Thyroid cancer survivors report poor quality of life after diagnosis and treatment compared with other patients who are diagnosed with more lethal cancers, according to new research from the University of Chicago Medicine.
The findings, published Dec. 11 in the journal Thyroid, shed light on a rarely studied outcome for a growing group of patients who are expected to soon account for 10 percent of all of American cancer survivors.
Thyroid cancer patients have a nearly 98 percent five-year survival rate, according to the National Cancer Institute. More than 95 percent survive a decade, leading some to call it a good cancer. But those successful outcomes mean few thyroid cancer survivorship studies have been conducted.
UChicago Medicine researchers Briseis Aschebrook-Kilfoy, PhD, assistant research professor in epidemiology, and Raymon Grogan, MD, assistant professor of surgery, are trying to address that data gap. Together, they lead the North American Thyroid Cancer Survivorship Study .
For their most recent research, Aschebrook-Kilfoy and Grogan recruited 1,174 thyroid cancer survivors 89.9 percent female with an average age of 48 from across the U.S. and Canada. Participants were recruited through the thyroid cancer clinics at UChicago Chicago Medicine, the clinics of six other universities, as well as through thyroid cancer survivor support groups and social media.
The researchers will continue to track participants to further understand this data.
Risk Factors For Thyroid Cancer
There are some things that can make it more likely to develop thyroid cancer. These are called risk factors and they include:
- Exposure to radiation a small number of thyroid cancers are due to having radiation therapy to the head and neck area as a child or living in an area with high levels of radiation.
- Family history only around 5% of thyroid cancer runs in families. Some inherited genetic conditions, such as familial adenomatous polyposis or Cowden syndrome, or inheriting the RET gene may also increase your risk.
- Other factors people who are overweight or obese possibly have a higher risk of developing thyroid cancer. Other thyroid conditions only slightly increase the chance of developing thyroid cancer.
Having these risk factors doesnt mean you will develop thyroid cancer. Often there is no clear reason for getting thyroid cancer. If you are worried about your risk factors, ask your doctor for advice.
What Is The Prognosis Of Papillary Thyroid Cancer
Overall, the prognosis of papillary thyroid cancer is excellent, especially if youre younger than 40 at diagnosis and have a small tumor. PTC can often be treated successfully and is rarely fatal, even if it has spread to lymph nodes in your neck.
Factors that may lead to a worse prognosis include:
- Being older than 55 years at diagnosis.
- Having a large tumor.
- If the cancer has spread to distant parts of your body.
- If you have a rare subtype of PTC, which are typically more aggressive, including the tall cell variant, diffuse sclerosis variant or solid variant.
Don’t Miss: When Should I Have My Thyroid Checked
Which Life Insurance Policy Type Is Best For Cancer Survivors
Most often, term life insurance for cancer survivors is the best option. It is the most affordable and provides coverage for a set number of years. However, depending on your needs, permanent life insurance, like whole life or universal life, may be the better choice. If you cant qualify, guaranteed acceptance life insurance, while more expensive, may be the only option available. Consider these policy types when choosing which is best for your situation.
A critical illness that requires immediate medical attention, such as a heart attack, stroke or cancer, can result in high medical bills. Critical illness coverage can provide a lump sum benefit to offset the medical costs associated with the diagnosis. It can also offer a death benefit to your chosen beneficiary if you pass away due to a critical illness. It can be combined with life insurance or purchased alone, though most carriers only offer it as an employee benefit, not a standalone policy.
Compare Life Insurance Rates
Ensure you are getting the best rate for your insurance. Compare quotes from the top insurance companies.
What Are The Warning Signs Of Thyroid Cancer
You or your healthcare provider might feel a lump or growth in your neck called a thyroid nodule. Donât panic if you have a thyroid nodule. Most nodules are benign . Only about 3 out of 20 thyroid nodules turn out to be cancerous .
Other thyroid cancer symptoms include:
- Difficulty breathing or swallowing.
- Swollen lymph nodes in your neck.
What are the signs that thyroid cancer has spread?
If you have thyroid cancer that has spread to other areas of your body, you may experience symptoms such as:
- Exposure to radioactive fallout from nuclear weapons or a power plant accident.
Read Also: Causes Of Thyroid Eye Disease
Prognostic Factors For Recurrent Disease
The 115 patients with a normal postablation TBS were followed up for a mean of 8 yr . The patient whose follow-up was less than 1 yr was excluded from further analysis.
The Tg/TSH at 612 months, available in 100 patients, was undetectable and detectable in 72 and 28 cases, respectively. Of note, the Tg level was less than 10 g/liter in 16 of the 28 patients with detectable Tg level. In the remaining 15 patients, either the recovery test was less than 80% or the Tg measurement was not performed .
Recurrences occurred in eight patients after a mean follow-up of 4.7 yr . Five- and 10-yr disease-free survivals were 96% and 91% , respectively. Recurrence occurred in neck LNs, lungs, and both lungs and thyroid bed in six, one, and one case, respectively. In these patients, the Tg/TSH level at 612 months was elevated in five patients, undetectable in two, and could not be measured because of interferences in one. The recurrences were found by neck palpation, diagnostic 131I TBS, and ultrasonography in six, one, and one case, respectively.
A New View Of Cancer Metastasis
In the lymph nodes, immune cells learn what to attack and what to protect .
But this study suggests that, in lymph nodes invaded by cancer, immune cells learn to protect the cancer cells rather than attack them, Dr. Engleman said. This phenomenon is called immune tolerance.
The research team suspects that those specialized cellsonce theyre educated by the tumorleave the lymph node, go all over the body, and instruct the immune system not to attack other cancer cells, he explained.
If thats the case, it would make distant organs more hospitable to the cancer, he said.
Thus, we propose a new model of metastasis we call Metastatic Tolerance, tweeted the studys lead scientist, Nathan Reticker-Flynn, Ph.D., of Stanford University.
Theres missing pieces about how exactly the T-regulatory cells get sent around the body, Dr. Dueck noted. But the idea is that there might be tolerance from the immune system by the time the cells get to distant organs.
With this new view of metastasis, the two prevailing theories on lymph nodes can be reconciled, Dr. Dueck explained. By spreading to lymph nodes and turning immune tolerance on, its easier for cancer cells in the primary tumor or in the lymph nodes to metastasize to distant organs.
Dr. Engleman and his team think it may be possible to develop therapies that switch off this tolerance. If used at the right time, such therapies could prevent cancer metastasis.
Don’t Miss: Thyroid Cancer 20 Year Survival Rate
What Are The Possible Side Effects And Complications Of Papillary Thyroid Cancer Treatment
Permanent hypothyroidism is an expected side effect of thyroidectomy and radioiodine therapy. Because of this, youll need to take replacement thyroid hormone medication for the rest of your life if you undergo either or both of these treatments.
Possible complications of thyroid surgery include:
- Accidental removal of or damage to your parathyroid glands, which help regulate your blood calcium levels.
- Damage to your recurrent laryngeal nerve, which runs behind your thyroid gland, resulting in hoarseness and a weak voice.
Potential side effects of radioactive iodine therapy include:
- Small risk of leukemia, breast or bladder cancer.
Prognosis And Survival Rates For Thyroid Cancer
When someone is diagnosed with thyroid cancer, their doctor will give them a prognosis. A prognosis is the doctors opinion of how likely the cancer will spread and the chances of getting better. A prognosis depends on the type and stage of cancer, test results and a persons age, fitness and medical history.
The most common types of thyroid cancer have an excellent long-term prognosis, especially if the cancer is found only in the thyroid or nearby lymph nodes in the neck. Even if the cancer has spread, the outcome can still be good.
Doctors commonly use 5-year survival rates as a way to discuss prognosis. This is because research studies often follow people for 5 years it does not mean you will survive for only 5 years. Thyroid cancer has a very high 5-year survival rate .
If you have thyroid cancer, your doctor will talk to you about your individual situation when working out your prognosis. Every persons experience is different, and there is support available to you.
Also Check: Do I Have To Fast For Thyroid Blood Test
Side Effects Of Thyroid Hormone Treatment
Thyroid hormone pills themselves do not usually cause side effects, but it can take some time to get the dosage right, and you may experience symptoms of either or while you and your doctor work to determine the correct dose.
Symptoms of too much thyroid hormone may include:
-
Increased heart rate
Symptoms of too little thyroid hormone may include:
-
dry skin and hair
Definitely check in with your doctor if you feel you are experiencing any of the above symptoms so that your dosage can be properly adjusted.
Cancer Cells Dodge Attack On The Way To Lymph Nodes
Next, the researchers asked what gives some melanoma cells the ability to spread to the lymph nodes.
They found that cancer cells that had spread to the lymph nodes had higher levels of certain proteins, including PD-L1 and MHC-I, than melanoma cells that didnt spread. High levels of PD-L1 and MHC-I send signals that tell cancer-fighting immune cells not to attack.
Further studies confirmed that higher levels of PD-L1 and MHC-I shielded melanoma cells from attack by immune cells. More specifically, immune cells called NK cells killed fewer melanoma cells that spread to the lymph nodes than melanoma cells that didnt spread.
Its quite remarkable what to dodge on the way to the lymph nodes. There is lots of immune attack, Dr. Engleman explained.
Read Also: What Are Some Symptoms Of Thyroid Cancer
General Information About Thyroid Cancer
In This Section
Thyroid cancer includes the following four main types:
For clinical management ofthe patient, thyroid cancer is generally divided into the following two categories:
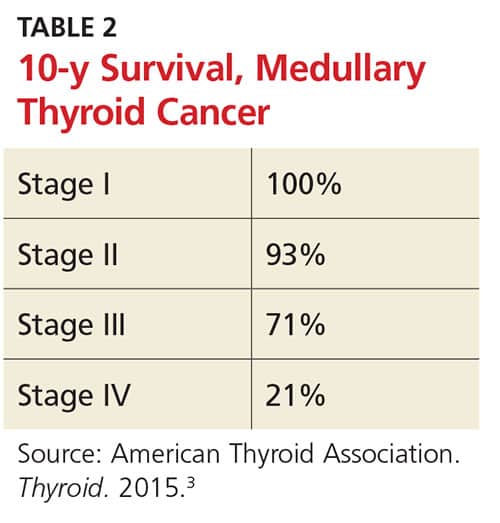
Well-differentiated tumors are highly treatable and usually curable. Poorly differentiated and undifferentiated thyroid tumors are less common, aggressive, metastasize early, and have a poorer prognosis. Medullary thyroid cancer is a neuroendocrine cancer that has an intermediate prognosis.
Thethyroid gland may occasionally be the site of other primary tumors, includingsarcomas, lymphomas, epidermoid carcinomas, and teratomas. The thyroid may also be the siteof metastasis from other cancers, particularly of the lung, breast, and kidney.
Life After Thyroid Cancer Surgery #3 Follow Up Lab Tests And Scans
The Clayman Thyroid Center believes that thyroid cancer patient follow-up is best managed by an endocrinologist with defined expertise in the evaluation, management, and follow-up of thyroid cancer patients. Communication between the endocrinologist, surgeon, radiologist, and other members of the thyroid cancer team is critical. This is the absolute foundation of thyroid cancer treatment at the Clayman Thyroid Center.
After thyroid cancer surgery, your thyroid hormone levels should be checked in 4-6 weeks to see if thyroid hormone medication is needed or if your dose should be adjusted. You should have a complete history and physical exam along with an expert ultrasound done 6 months after thyroid cancer surgery and yearly after that. The following blood tests are always done routinely for surveillance and monitoring:
1) Free T4 level: This is the blood level of the major hormone normally produced by the thyroid gland. This is also a direct measurement of the most commonly prescribed thyroid hormone pill, levothyroxine or Synthroid. The dose of thyroid hormone pill will be based upon the blood thyroid stimulating hormone level described below.
Additional blood tests that are used to monitor medullary thyroid cancer are calcitonin and CEA .
A PET/CT scan in a patient with thyroid cancer spread to the lungs is seen below.
Check out this post for more information regarding staging and imaging for thyroid cancer along with follow-up.
You May Like: Does Medicare Cover Thyroid Ultrasound
Kaplanmeier Analyses Of Disease
On the analysis of disease-specific survival of all TC patients, NX was associated with a statistically significant decrease in survival, followed by N1NOS and N1b groups, while N1a and N0 showed better survival . In PTC, The NX group had the poorest survival with a sharp decrease, followed by N1b, N1a, and N0 groups, while N1NOS groups had better survival . In FTC, the worst survival was obtained in the N1NOS group, followed by N1a and N1b groups with a sharp decrease, while N0 and NX groups had better survival . There was no statistically significant decrease in MTC . In ATC, the N stage had no significant effect on disease-specific survival .
Figure 1. Disease specific survival of TC patients stratified by N stage using Kaplan-Meier analysis.
Figure 2. Disease specific survival of PTC patients stratified by N stage using Kaplan-Meier analysis.
Figure 3. Disease specific survival of FTC patients stratified by N stage using Kaplan-Meier analysis.
Figure 4. Disease specific survival of MTC patients stratified by N stage using Kaplan-Meier analysis.
Figure 5. Disease specific survival of ATC patients stratified by N stage using Kaplan-Meier analysis.
Papillary Thyroid Cancer Quick Facts:
- Peak onset ages 30 through 50
- Females more common than males by 3 to 1 ratio
- Prognosis directly related to tumor size
- Accounts for 85% of thyroid cancers
- Can be caused by radiation or x-ray exposure
- Spread to lymph nodes of the neck present in up to 50% of cases
- Distant spread is very rare
- Overall cure rate very high
Don’t Miss: What Vitamins Are Good For Your Thyroid
Characteristics Of Papillary Thyroid Cancer
-
Peak onset ages are 30 to 50 years old.
-
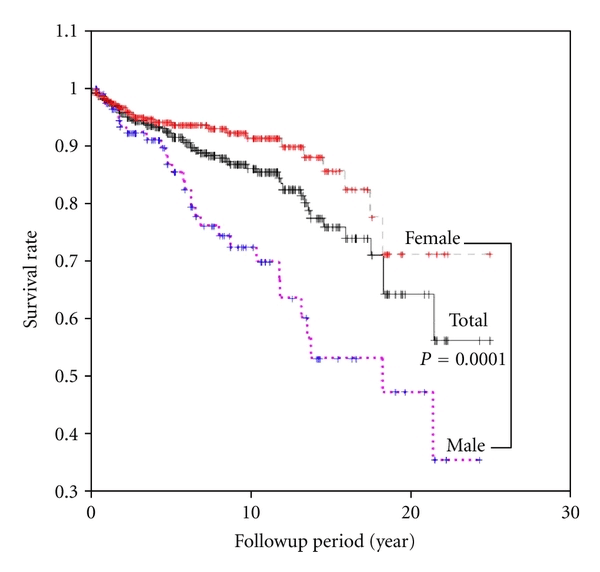
Papillary thyroid cancer is more common in females than in males by a 3:1 ratio.
-
The prognosis is directly related to tumor size. Less than 1.5 cm is a good prognosis.
-
The prognosis is also directly related to age. Patients under 55 years of age do much better than patients who are over 55 years of age.
-
The prognosis is directly related to gender. Women have a much better prognosis than do similarly aged men.
-
This cancer accounts for 85% of thyroid cancers due to .
-
In more than 50% of cases, it spreads to lymph nodes of the neck.
-
Distant spread is uncommon.
-
The overall cure rate is very high .Management of Papillary Thyroid Cancer
Considerable controversy exists when discussing the management of well-differentiated thyroid carcinomasboth papillary thyroid cancer and even follicular thyroid cancer.
Some experts contend that if these tumors are small and not invading other tissues then simply removing the lobe of the thyroid that harbors the tumor will provide as good a chance of cure as removing the entire thyroid.
These proponents of conservative surgical therapy relate the low rate of clinical tumor recurrence despite the fact that small amounts of tumor cells can be found in up to 88% of the opposite lobe thyroid tissues. They also cite some studies showing an increased risk of and recurrent laryngeal nerve injury in patients undergoing total thyroidectomy .
Thyroid Cancer Surgery On Lymph Nodes
The lymph nodes of the body function similar to a charcoal filter system. Thyroid cancer cells can get caught within the filter but the body has no means of removing the captured cells. The cells are basically then stuck in the lymph node and they begin to grow in that location. The lymph node areas of the neck can be divided into three basic areas:
Thyroid cancer surgery must address the lymph node areas that are known to contain cancer as well as those that are at significant risk of having thyroid cancer. This type of the thyroid cancer surgery is termed comprehensive compartmental dissection.
Comprehensive does not mean destructive by any means. These lymph node surgeries remove lymph nodes and fatty tissue and spare all major nerves, blood vessels and muscles. They have essentially no cosmetic or functional impact other than a fine scar line.
The two types of comprehensive compartmental dissections which we will discuss here are:
Recommended Reading: How To Control Thyroid In Female By Food
Side Effects Of Thyroid Surgery
The risks of thyroid surgery include:
-
Damage to the laryngeal nerve. It can be stunned, or one vocal cord wont move the same way as the other, Dr. Harari explains. About 5% of people temporarily experience this complication, and 1% have permanent damage. There are procedures to regain vocal strength, and an ENT specialist can assist the patient in these efforts.
-
Hypoparathyroidism, or, as sometimes surgeons decide to remove one or more of the parathyroid glands four tiny glands that regulate the bodys calcium levels and are located near the back of the thyroid. People whose thyroid surgery involves a central neck incision have a 10% risk of parathyroid complications.
-
Vagus nerve issues. Lateral neck incisions can risk impacting the vagus nerve, Dr. Harari says. This can have effects on the voice as well as the shoulder or tongue.
-
Loss of thyroid function. After surgery, you will probably need to take pills for the rest of your life to replace lost thyroid hormones. If your parathyroid glands are also removed, you may also need to take calcium and vitamin D.