Thyroid Nodules And Cancer During Pregnancy
American Thyroid Association guidelines on management of thyroid disease during pregnancy and the postpartum include the following recommendations on thyroid nodules and cancer in these patients :
Recommendations for subsequent pregnancy in women with thyroid cancer include the following:
- Pregnancy should be deferred for 6 months after a woman has received therapeutic radioactive iodine treatment.
- In women with thyroid cancer who become pregnant, the TSH goal should remain the same as determined preconception. TSH should be monitored approximately every 4 weeks until 1620 weeks of gestation, and at least once between 26 and 32 weeks of gestation.
- Women with previously treated differentiated thyroid cancer who have undetectable serum thyroglobulin levels and are classified as having no biochemical or structural evidence of disease prior to pregnancy do not require ultrasound and Tg monitoring during pregnancy.
- Women diagnosed with papillary thyroid microcarcinoma who are under active surveillance should have ultrasound monitoring of their thyroid performed each trimester during pregnancy.
References
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016 Jan. 26 :1-133. . .
Living As A Thyroid Cancer Survivor
For many people with thyroid cancer, treatment may remove or destroy the cancer. Completing treatment can be both stressful and exciting. You may be relieved to finish treatment, but find it hard not to worry about cancer growing or coming back. This is very common concern if you have had cancer.
For other people, thyroid cancer may never go away completely, or it might come back in another part of the body. These people may get regular treatments with chemotherapy, radiation therapy, or other therapies to help keep the cancer under control for as long as possible. Learning to live with cancer that does not go away can be difficult and very stressful.
Low Risk Tumors Represent The Majority Of Dtc
Contemporary longitudinal cohorts of DTC patients consist of low-risk tumors by roughly two-thirds .
Another category of patients with excellent prognosis are intrathyroidal and have unifocal PTC of 10 mm or less, with no local or distant metastases, no aggressive histologic variant, and no history of familial non-medullary thyroid cancer or head and neck radiotherapy in childhood . These tumors have an excellent prognosis with or without radioiodine treatment and when excellent response is achieved the risk of recurrence is virtually zero . These very low-risk PTC represent about two out of three of all PTC of 10 mm or less and a considerable percentage of all DTCs .
The costs of surveillance of this growing number of low-risk DTC are important. With regard to the healthcare system, it has been estimated that the cost of one recurrence diagnosis in low risk was six and seven times greater than in intermediate and high-risk patients, respectively . Moreover, a hidden social cost in terms of patient anxiety and depression is emerging in thyroid cancer patients despite a good prognosis and thyroid cancer is recognized as a cause of patient financial bankruptcy .
In this context, the issue of effective management of low-risk DTC and a possible end of life-long surveillance is a priority.
The absence of abnormal findings on neck US coupled with TSH-stimulated serum Tg < 1 ng/mL, in the absence of TgAbs, has a negative predictive value approaching 100% .
Also Check: What To Do To Help Thyroid Problems
Treatment Of Anaplastic Thyroid Cancer
As with many other aggressive cancers, the treatment approach for anaplastic thyroid cancer has benefited from a better understanding of specific tumor characteristics and the development of targeted chemotherapeutics. Given the aggressive nature and relatively poor outcomes with this cancer, guidelines recommend a prompt evaluation of tumor and a multidisciplinary discussion with surgeons, oncologists, palliative care specialists, and the patient. In particular, the potential for rapid airway and vascular compromise make early evaluation critical.
For staging, patient should undergo fluorodeoxyglucose PET/CT or dedicated body CT or MRI. Patients with stage IVA or IVB disease who wish to pursue surgery can undergo complete resection with early adjuvant therapy to follow. Importantly, surgical planning must take into account the need to limit wounds that might lead to complications that would prevent early chemotherapy and radiation therapy. Following surgery for stage IVA/IVB disease, patients should undergo definitive-intention radiation therapy with chemotherapy .
Patients with stage IVC ATC can also opt for early palliative chemotherapy and/or radiation, as they will not be candidates for surgical resection. Close communication with patients and their family is important in these cases, as many individual factors may enter into the choice between palliative therapies or more aggressive care.
What Is The Follow
Periodic follow-up examinations are essential for all patients with thyroid cancer, because the thyroid cancer can returnsometimes several years after successful initial treatment. These follow-up visits include a careful history and physical examination, with particular attention to the neck area. Neck ultrasound is an important tool to view the neck and look for nodules, lumps or cancerous lymph nodes that might indicate the cancer has returned. Blood tests are also important for thyroid cancer patients. Most patients who have had a thyroidectomy for cancer require thyroid hormone replacement with levothyroxine once the thyroid is removed . The dose of levothyroxine prescribed by your doctor will in part be determined by the initial extent of your thyroid cancer. More advanced cancers usually require higher doses of levothyroxine to suppress TSH . In cases of minimal or very low risk thyroid cancer, it is typically recommended to keep TSH in the normal range. The TSH level is a good indicator of whether the levothyroxine dose is correct and should be followed periodically by your doctor.
In addition to routine blood tests, your doctor may want to check a whole-body iodine scan to determine if any thyroid cancer cells remain. These scans are only done for high risk patients and have been largely replaced by routine neck ultrasound and thyroglobulin measurements that are more accurate to detect cancer recurrence, especially when done together.
Don’t Miss: How Do I Get My Thyroid Tested
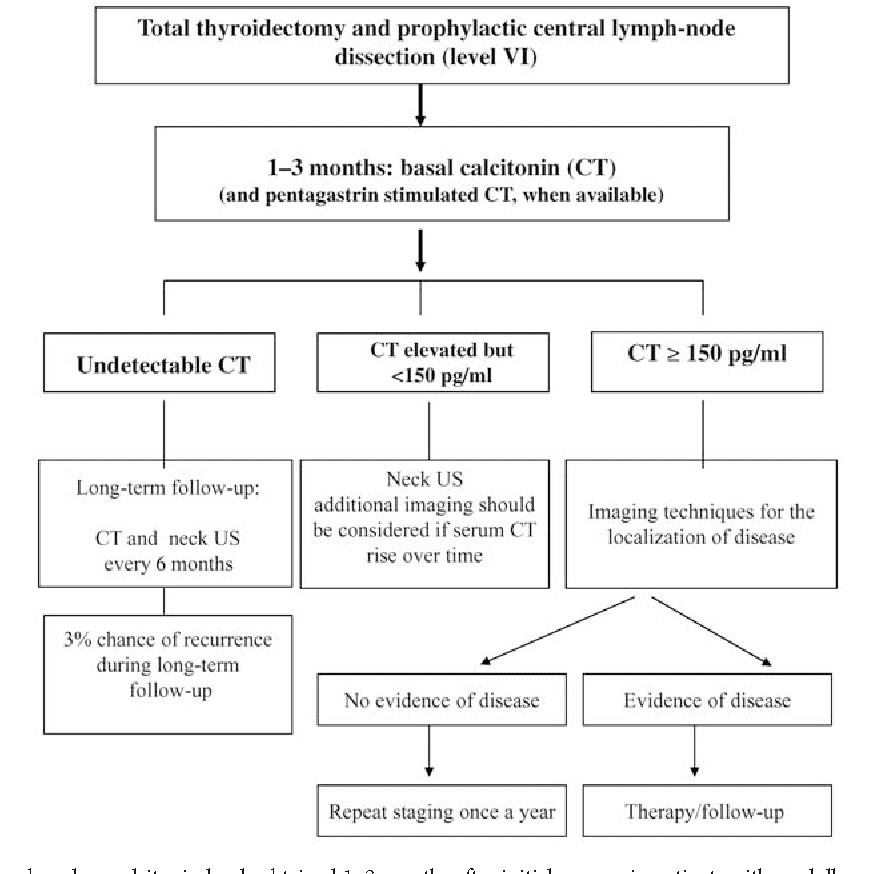
Prevention Of Medullary Thyroid Cancer
The familial medullary thyroid carcinoma syndromes consist of multiple endocrine neoplasia types 2A and 2B and familial MTC. They are inherited in an autosomal dominant fashion. Children inheriting any of these syndromes have a 100% risk of developing MTC. In MEN 2B, MTC usually develops around 10 years of age and has a high propensity for rapid growth and metastasis. In MEN 2A, MTC can appear in the first decade of life, and it almost always develops by the second decade. MTC in FMTC usually develops during adulthood.
Guidelines from the American Thyroid Association and NCCN recommend prophylactic thyroidectomy for individuals that have a documented RET mutation and are at risk for aggressive MTC. Risk varies with the underlying RET mutation.
The original ATA guidelines, from 2009, stratified risk level of RET carriers into four categories, A through D, based upon the increasing aggressiveness of the particular mutation. Due to some confusion and lack of uniformity with other staging guidelines, the revised ATA guidelines, published in 2015, transition category D to highest risk , transition category C to high risk , and combine categories B and A into moderate risk. The risk stratification, screening schedules, and prophylactic thyroidectomy schedules are described in the table below.
Table. American Thyroid Association Medullary Thyroid Cancer Risk Levels and Treatment Recommendations
Can Rhtsh Be Used As An Alternative To Thyroxine Withdrawal For Remnant Ablation Or Adjuvant Therapy In Patients Who Have Undergone Near
â RECOMMENDATION 54
In patients with ATA low-risk and ATA intermediate-risk DTC without extensive lymph node involvement , in whom RAI remnant ablation or adjuvant therapy is planned, preparation with rhTSH stimulation is an acceptable alternative to thyroid hormone withdrawal for achieving remnant ablation, based on evidence of superior short-term quality of life, noninferiority of remnant ablation efficacy, and multiple consistent observations suggesting no significant difference in long-term outcomes.
In patients with ATA intermediate-risk DTC who have extensive lymph node disease in the absence of distant metastases, preparation with rhTSH stimulation may be considered as an alternative to thyroid hormone withdrawal prior to adjuvant RAI treatment.
In patients with ATA high-risk DTC with attendant higher risks of disease-related mortality and morbidity, more controlled data from long-term outcome studies are needed before rhTSH preparation for RAI adjuvant treatment can be recommended.
In patients with DTC of any risk level with significant comorbidity that may preclude thyroid hormone withdrawal prior to iodine RAI administration, rhTSH preparation should be considered. Significant comorbidity may include a significant medical or psychiatric condition that could be acutely exacerbated with hypothyroidism, leading to a serious adverse event, or inability to mount an adequate endogenous TSH response with thyroid hormone withdrawal.
You May Like: Stop The Thyroid Madness Com
Goals Of Initial Therapy Of Dtc
The basic goals of initial therapy for patients with DTC are to improve overall and disease-specific survival, reduce the risk of persistent/recurrent disease and associated morbidity, and permit accurate disease staging and risk stratification, while minimizing treatment-related morbidity and unnecessary therapy. The specific goals of initial therapy are to
What Is The Prognosis Of Thyroid Cancer
Overall, your prognosis with differentiated thyroid cancer is excellent, especially if you are younger than 55 years of age and have a small cancer. If your papillary thyroid cancer has not spread beyond the thyroid gland, patients like you rarely if ever die from thyroid cancer. If you are older than 55 years of age, or have a larger or more aggressive tumor, your prognosis remains very good, but the risk of cancer recurrence is higher. The prognosis may not be quite as good if your cancer is more advanced and cannot be completely removed with surgery or destroyed with radioactive iodine treatment. Nonetheless, even if this is your situation, you will likely be able to live a long time and feel well, despite the fact that you are living with cancer. It is important to talk to your doctor about your individual profile of cancer and expected prognosis. It will be necessary to have lifelong monitoring, even after successful treatment.
Also Check: Only Natural Pet Feline Thyroid Wellness
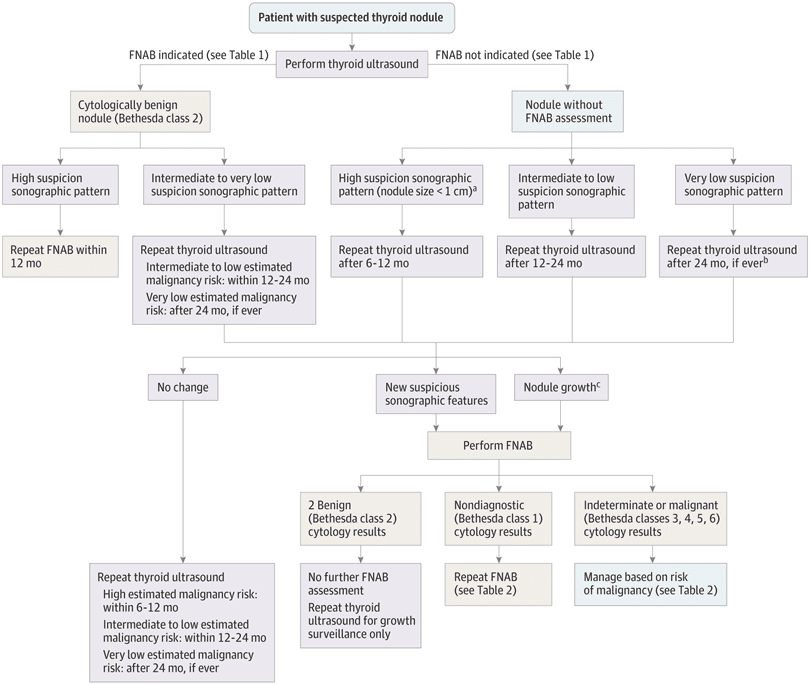
What Are The Best Methods For Long
Recommendations for initial follow-up of nodules with benign FNA cytology
â RECOMMENDATION 23
Given the low false-negative rate of US-guided FNA cytology and the higher yield of missed malignancies based upon nodule sonographic pattern rather than growth, the follow-up of thyroid nodules with benign cytology diagnoses should be determined by risk stratification based upon US pattern.
Nodules with high suspicion US pattern: repeat US and US-guided FNA within 12 months.
Nodules with low to intermediate suspicion US pattern: repeat US at 12â24 months. If sonographic evidence of growth or development of new suspicious sonographic features, the FNA could be repeated or observation continued with repeat US, with repeat FNA in case of continued growth.
Nodules with very low suspicion US pattern : the utility of surveillance US and assessment of nodule growth as an indicator for repeat FNA to detect a missed malignancy is limited. If US is repeated, it should be done at â¥24 months.
Recommendation for follow-up of nodules with two benign FNA cytology results
If a nodule has undergone repeat US-guided FNA with a second benign cytology result, US surveillance for this nodule for continued risk of malignancy is no longer indicated.
Follow-up for nodules that do not meet FNA criteria
â RECOMMENDATION 24
Nodules with high suspicion US pattern: repeat US in 6â12 months.
Nodules with low to intermediate suspicion US pattern: consider repeat US at 12â24 months.
Ask Your Doctor For A Survivorship Care Plan
Talk with your doctor about developing a survivorship care plan for you. This plan might include:
- A suggested schedule for follow-up exams and tests
- A list of possible late- or long-term side effects from your treatment, including what to watch for and when you should contact your doctor
- A schedule for other tests you might need, such as early detection tests for other types of cancer, or test to look for long-term health effects from your cancer or its treatment
- Diet and physical activity suggestions that might improve your health, including possibly lowering your chances of the cancer coming back
- Reminders to keep your appointments with your primary care provider , who will monitor your general health care
Read Also: Best Thyroid Diet To Lose Weight
Absence Of Rai Uptake In Some But Not All Lesions
Although a mixed pattern with some lesions accumulating RAI and others not is also considered RAI refractory disease in most publications, it is uncertain whether this is correct, as no study has shown that continuation of RAI treatment in this situation is not beneficial. A combination of RAI therapy for RAI-avid lesions and local treatment for one or a limited number of RAI refractory lesions may be considered in certain patients.
What Causes Thyroid Cancer
Thyroid cancer is more common in people who have a history of exposure to high doses of radiation, have a family history of thyroid cancer, and are older than 40 years of age. However, for most people, we dont know why thyroid cancer develops.
High dose radiation exposure, especially during childhood, increases the risk of developing thyroid cancer. Radiation therapy used to treat cancers such as Hodgkins disease or breast cancer has been associated with an increased risk for developing thyroid cancer if the treatment included exposure to the head, neck or chest. Routine X-ray exposure such as dental X-rays, chest X-rays and mammograms are not associated with a high risk of thyroid cancer. As always, you should minimize radiation exposure by only having tests which are medically necessary.
Exposure to radioactivity released during nuclear disasters has also been associated with an increased risk of developing thyroid cancer, particularly in exposed children, and thyroid cancers can be seen in exposed individuals as many as 40 years after exposure.
Read Also: How To Treat Thyroid Problems In Humans
What Are The Principles Of The Molecular Testing Of Fna Samples
Molecular markers may be classified according to intended use that is, diagnostic , prognostic, or predictive purposes . Furthermore, companion use of predictive molecular markers involves the identification of patient subgroups in which a therapeutic intervention is proven to be either beneficial or harmful, with intended implications for appropriate clinical stratification of therapies . Validation studies of molecular marker tests may include examination of analytic validity , clinical validity , and clinical utility . Furthermore, an NCCN Tumor Marker Task Force has indicated that the clinical utility of a molecular test should be founded in strong evidence proving that use of the marker âimproves patient outcomes sufficiently to justify its incorporation into routine clinical practice.ââ
A number of molecular approaches have been studied in the clinical setting of indeterminate FNA cytologic interpretation . One could surmise that an ideal ârule-inâ test would have a PPV for histopathologically proven malignancy similar to a malignant cytologic diagnosis , and an ideal ârule-outâ test would have a NPV similar to a benign cytologic diagnosis , and these would hold true with a reasonable degree of precision and reproducibility.
â RECOMMENDATION 13
â RECOMMENDATION 14
AUS/FLUS cytology
â RECOMMENDATION 15
Follicular neoplasm/suspicious for follicular neoplasm cytology
â RECOMMENDATION 16
Suspicious for malignancy cytology
â RECOMMENDATION 17
Diagnostic Tools Limitations And Gray Zone Responses
TgAbs are found in about 20% of DTC patients . False-negative and, less frequently false-positive, Tg results can occur in the presence of TgAbs using common laboratory immunometric or radioimmunometric assays . The use of mass spectrometry may overcome this limitation, but the results obtained in real-life clinical practice are less convincing than those obtained in an experimental setting . A stable or declining trend of serum TgAbs over time is associated with disease remission , nonetheless these patients cannot be classified as excellent response until TgAb become negative .
The positive predictive value of Tg is poor. Persistence of detectable serum Tg in the absence of suspicious findings on imaging is found in about 20% of low-risk DTCs . This situation is called biochemical-incomplete response or indeterminate response to treatment .
Patients with rising levels of TgAbs over time in the absence of suspicious findings are considered as biochemical-incomplete response and the presence of stable or declining titers of TgAbs in the absence of suspicious findings on imaging is considered as an indeterminate response to treatment .
Only 36% and 11% of low-risk DTC patients with biochemical-incomplete and indeterminate response will develop structural disease, respectively , and Tg will spontaneously decrease to undetectable values fulfilling the definition of excellent response in a percentage between 50 and 80% of these patients.
Read Also: Treatment Of Medullary Thyroid Cancer
Development Of Management Plans
Based on the above-mentioned information, integral management plans can be designed, not only focussing on medical management , but also addressing the social, emotional, and spiritual needs of the patient. The problem with developing medical plans is that there is limited evidence based on clinical studies that can be translated directly to the situation of the individual patient. As a consequence, developing these plans is based mostly on expert opinion and the experience of a MDT in which all healthcare specialists are represented, not restricted to medical specialists, but also general practitioners, social, psychological, and spiritual caregivers.
Doctor Visits And Follow
Your health care team will explain what tests you need and how often they should be done. Your schedule of doctor visits, exams, and tests will depend on the original extent of your cancer, the specific type of thyroid cancer you had, how it was treated, and other factors.
Papillary or follicular cancer: If you have had papillary or follicular cancer, and your thyroid gland has been completely removed or ablated, your doctors may consider at least one radioactive iodine scan after treatment, especially if you are at higher risk for recurrence. This is usually done about 6 to 12 months later. If the result is negative, you will generally not need further scans unless you have symptoms or other abnormal test results.
Your blood will also be tested regularly for TSH and thyroglobulin levels. Thyroglobulin is made by thyroid tissue, so after total thyroid removal and ablation it should be at very low levels or not be found in your blood at all. If the thyroglobulin level begins to rise, it might be a sign the cancer is coming back, and further testing will be done. This usually includes a radioactive iodine scan, and may include PET scans and other imaging tests.
For those with a low-risk, small papillary cancer that was treated by removing only one lobe of the thyroid, routine physical exams by your doctor, thyroid ultrasounds and thyroid blood tests are typical.
You May Like: If Thyroid Levels Are High