Treatment For Differentiated Thyroid Cancer
At CHOP, experts at the Pediatric Thyroid Center take a team approach to treatment for children with differentiated thyroid cancer. Our board-certified team of endocrinologists, oncologists, pediatric surgeons, pathologists, radiologists and nurses collaborate to provide your child with individualized care and the best possible outcome.
Our Center is led by Andrew J. Bauer, MD, a world-renowned endocrinologist and researcher, who is often sought for second opinions on difficult-to-diagnose thyroid disorders. Dr. Bauer is a member of the American Thyroid Association and co-chaired an international ATA task force that created the first guidelines for evaluating and managing thyroid nodules and thyroid cancer in children.
Thyroid cancer is treated with surgery and radioactive iodine. At Childrens Hospital, our clinicians have the expertise to determine whether your child needs more or less extensive surgery, and a single or repeated doses of radioactive iodine. These decisions can reduce complication rates and optimize immediate and long-term quality of life for your child.
Clinicians from the Pediatric Thyroid Center will discuss the treatment plan with your child and family, and explain what to expect before, during and after surgery. The team will also detail when your child should begin a low-iodine diet, stop thyroid hormone therapy, and when radioactive iodine whole body scans and treatment may begin.
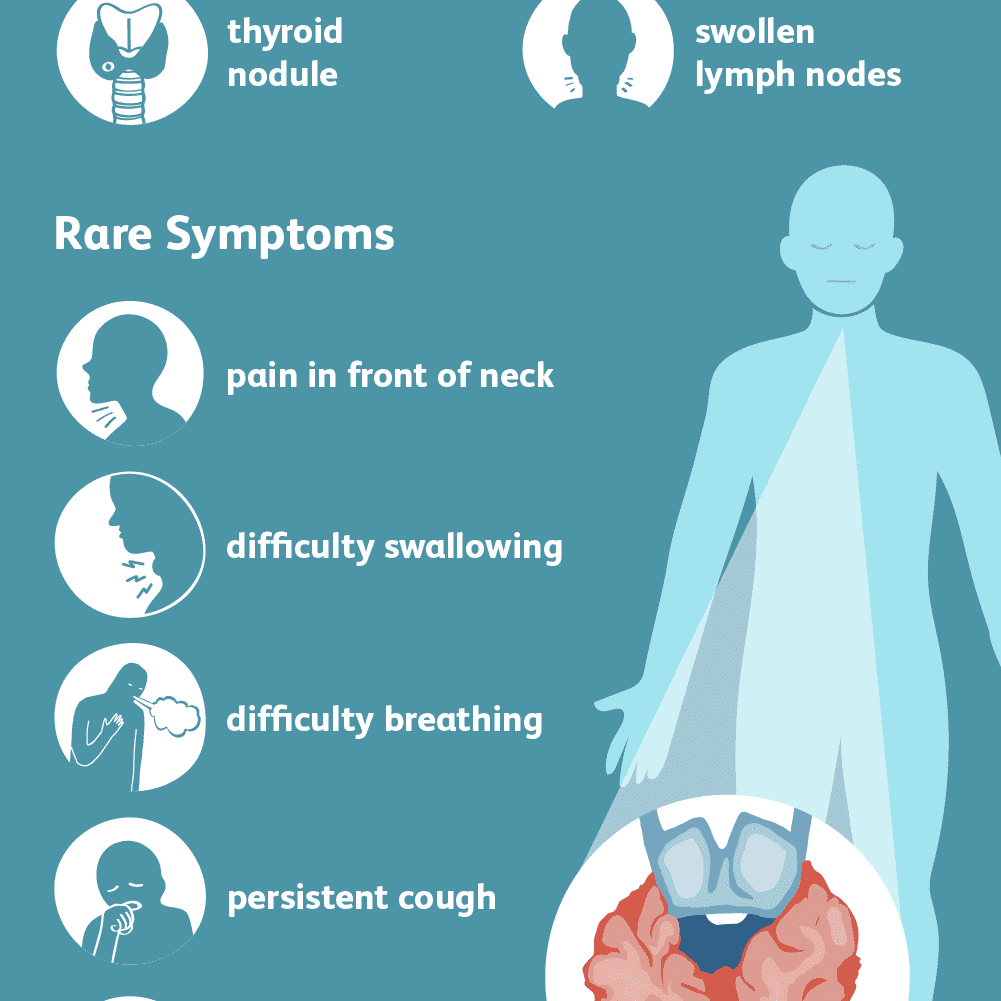
Signs And Symptoms Of Thyroid Cancer
Thyroid cancer can cause any of the following signs or symptoms:
- A lump in the neck, sometimes growing quickly
- Swelling in the neck
- Pain in the front of the neck, sometimes going up to the ears
- Hoarseness or other voice changes that do not go away
- Trouble swallowing
- Trouble breathing
- A constant cough that is not due to a cold
If you have any of these signs or symptoms, talk to your doctor right away. Many of these symptoms can also be caused by non-cancerous conditions or even other cancers of the neck area. Lumps in the thyroid are common and are usually benign. Still, if you have any of these symptoms, its important to see your doctor so the cause can be found and treated, if needed.
Our team is made up of doctors and oncology certified nurses with deep knowledge of cancer care as well as journalists, editors, and translators with extensive experience in medical writing.
Davidge-Pitts CJ and Thompson GB. Chapter 82: Thyroid Tumors. In: DeVita VT, Lawrence TS, Rosenberg SA, eds. DeVita, Hellman, and RosenbergsCancer: Principles and Practice of Oncology. 10th ed. Philadelphia, Pa: Lippincott Williams & Wilkins 2015.
National Cancer Institute. Physician Data Query . Thyroid Cancer Treatment. 05/23/2018. Accessed at https://www.cancer.gov/types/thyroid/patient/thyroid-treatment-pdq#_1. on February 20, 2019.
Last Revised: March 14, 2019
What Causes Thyroid Cancer In Children
The vast majority of thyroid cancers in children have no known cause. However, there are some known risk factors for developing thyroid cancer, including radiation exposure and certain genetic conditions.
What causes some children to develop thyroid nodules and thyroid cancer is an area of active in our .
Read Also: Foods That Fight Thyroid Cancer
Thyroid Nodules May Be Found During A Routine Medical Exam And Are Usually Not Cancer
Your childs doctor may find a lump in the thyroid during a routine medical exam, or a nodule may be seen on an imaging test or during surgery for another condition. A thyroid nodule is an abnormal growth of thyroid cells in the thyroid. Nodules may be solid or fluid-filled.
When a thyroid nodule is found, an ultrasound of the thyroid and lymph nodes in the neck is done. A fine-needle aspiration biopsy may be done to check for signs of cancer. Blood tests to check thyroid hormone levels and for anti-thyroid antibodies in the blood may also be done. This is to check for other types of thyroid disease.
Thyroid nodules usually don’t cause symptoms or need treatment. Sometimes the thyroid nodules become large enough that it is hard to swallow or breathe and more tests and treatment are needed. Only one in five thyroid nodules become cancer.
Outlook For Thyroid Cancer
Around 9 in every 10 people are alive 5 years after a diagnosis of thyroid cancer. Many of these are cured and will have a normal lifespan.
But the outlook varies depending on the type of thyroid cancer and how early it was diagnosed. At present the outlook is:
- more than 9 in 10 people with papillary carcinoma live at least 5 years after diagnosis
- more than 9 in 10 people with follicular carcinoma live at least 5 years after diagnosis
- more than 7 in 10 men, and around 9 in 10 women with medullary thyroid carcinoma live at least 5 years after diagnosis
- around 1 in 10 people with anaplastic thyroid carcinoma live at least 5 years after diagnosis
Up to 1 in 4 people treated for thyroid cancer are later diagnosed with cancer in another part of the body, such as the lungs or bones, but cancer can often be treated again if this happens.
Page last reviewed: 28 August 2019 Next review due: 28 August 2022
Recommended Reading: Can You Lose Weight With Thyroid Issues
How Is Thyroid Cancer Managed Or Treated
Treatments for thyroid cancer depend on the tumor size and whether the cancer has spread. Treatments include:
- Surgery: Surgery is the most common treatment for thyroid cancer. Depending on the tumorâs size and location, a surgeon may remove part of your thyroid gland or all of the gland . The surgeon also removes any nearby lymph nodes where cancer cells have spread.
- Radioiodine therapy: With radioiodine therapy, you swallow a pill or liquid containing a higher dose of radioactive iodine than whatâs used in a diagnostic radioiodine scan. The radioiodine shrinks and destroys the diseased thyroid gland along with cancer cells. This treatment is very safe. Your thyroid gland absorbs almost all of the radioiodine and the rest of your body has minimal radiation exposure.
- Radiation therapy: Radiation kills cancer cells and stops them from growing. External radiation therapy uses a machine to deliver strong beams of energy directly to the tumor site. Internal radiation therapy involves placing radioactive seeds in or around the tumor.
- Chemotherapy: Intravenous or oral chemotherapy drugs kill cancer cells and stops cancer growth. Very few people diagnosed with thyroid cancer will ever need chemotherapy.
- Hormone therapy: This treatment blocks the release of hormones that can cause cancer to spread or come back.
What are the complications of thyroid cancer?
How does thyroid cancer affect pregnancy?
What Are The Types Of Pediatric Thyroid Cancer
PapillaryThis form of thyroid cancer occurs in cells that produce thyroid hormones containing iodine. This type, the most common form of thyroid cancer in children, grows very slowly. This form can spread to the lymph nodes via lymphatics in the neck and occasionally spreads to more distant sites.
FollicularThis type of thyroid cancer also develops in cells that produce thyroid hormones containing iodine. The disease afflicts a slightly older age group and is less common in children. This type of thyroid cancer is more likely to spread to the neck via blood vessels, causing the cancer to spread to other parts of the body, making the disease more difficult to control.
MedullaryThis rare form of thyroid cancer develops in cells that produce calcitonin, a hormone that does not contain iodine. This cancer tends to spread to other parts of the body and constitutes about five- to 10-percent of all thyroid malignancies. Medullary thyroid carcinoma in the pediatric population is usually associated with specific inherited genetic conditions, such as multiple endocrine neoplasia type 2 .
AnaplasticThis is the fastest growing of the thyroid cancers, with abnormal cells that grow and spread rapidly, especially locally in the neck. This form of cancer is not seen in children.
css id:
Don’t Miss: Thyroid Saliva Test At Home
Medullary Thyroid Cancer Is Sometimes Caused By A Change In A Gene That Is Passed From Parent To Child
The genes in cells carry hereditary information from parent to child. A certain change in the RET gene that is passed from parent to child may cause medullary thyroid cancer.
There is a genetic test that is used to check for the changed gene. The patient is tested first to see if he or she has the changed gene. If the patient has it, other family members may also be tested to find out if they have an increased risk of medullary thyroid cancer. Family members, including young children, who have the changed gene may have a thyroidectomy . This can decrease the chance of developing medullary thyroid cancer.
Men2b Syndrome Causes Several Conditions
Patients with MEN2B syndrome may have a slender body build with long, thin arms and legs. The lips may appear large and bumpy because of benign tumors in the mucous membranes. MEN2B syndrome may cause the following conditions:
- Medullary thyroid cancer .
- Pheochromocytoma.
- Nerve cell tumors in the mucous membranes or other places.
The prognosis for MEN2B syndrome is not as good as the prognosis for MEN1 syndrome and MEN2A syndrome because medullary thyroid cancer is a more aggressive cancer.
Don’t Miss: Is Vitamin C Good For Thyroid Patients
What Are The Symptoms Of Pediatric Thyroid Cancer
Symptoms of this disease vary. Your child may experience:
- A lump in the neck
- Persistent swollen lymph nodes
- A tight or full feeling in the neck
- Trouble with breathing or swallowing
If any of these symptoms occur, consult your childs physician for an evaluation. The evaluation should consist of a head and neck examination to determine if unusual lumps are present. A blood test may be ordered to determine how the thyroid is functioning. Ultrasonography uses sound waves to create an image of the thyroid gland and neck contents such as lymph nodes.
Other tests that may be warranted include a radioactive iodine scan, which provides information about the thyroid shape and function and identifies areas in the thyroid that do not absorb iodine in the normal way, or a fine needle biopsy of any abnormal lump in the thyroid or neck. Also called fine needle aspiration , a fine needle biopsy is when a needle is inserted into a lump or mass to collect a sample of cells. Sometimes it is necessary to remove a part of the tumor or one of the lobes of the thyroid gland, known as a thyroid lobectomy, for analysis to help establish a diagnosis and plan for management..
css id:
When To See A Doctor
Thyroid issues are often hereditary, so if you have a family history of these conditions, talk to your pediatrician about how often you should schedule thyroid disease screening tests for your child.
If you notice that he or she has symptoms of hyperthyroidism or hypothyroidism, make a doctor’s appointment so that the cause can be identified and treated.
Your child’s doctor will likely order blood tests that include thyroid hormone levels:
- Children with hypothyroidism may have a low free thyroxine level and an elevated level of thyroid stimulating hormone .
- Children with hyperthyroidism will usually have a high T4 and triiodothyronine and a low TSH.
She may also order imaging studies or diagnostic tests to rule out other conditions as well.
Thyroid Disease Doctor Discussion Guide
Get our printable guide for your next doctor’s appointment to help you ask the right questions.
Don’t Miss: How To Control Thyroid In Female By Food
If Cancer Such As Medullary Thyroid Cancer Has Formed Tests Are Done To Find Out If Cancer Cells Have Spread To Nearby Areas Or To Other Parts Of The Body
The process used to find out if cancer has spread to nearby areas or to other parts of the body is called staging. There is no standard system for staging childhood cancers linked to MEN syndromes. The results of the tests and procedures done to diagnose cancer are used to help make decisions about treatment.
Sometimes childhood MEN syndromes recur after treatment.
Radioactive Iodine Ablation And Therapy
Typically, there is remnant thyroid tissue after a total or near-total thyroidectomy, mainly because of the presence of normal thyroid tissue around the nerves or Berrys ligament. Because multifocal papillary cancer is relatively common in children, most authors recommend radioiodine ablation therapy in younger patients . Ablation therapy presumably not only destroys normal residual thyroid tissue but also possible micrometastases . Moreover, follow-up Tg measurement is easier after radioiodine ablation therapy . In other words, if a patient receives radioiodine ablation therapy and the Tg level reaches an undetectable level, a subsequent rise in Tg level is highly suspicious of recurrence. In contrast, a rise in Tg level in a patient who did not receive ablation therapy may be the result of tumor recurrence or the regrowth of normal thyroid tissue . In the majority of cases, a single radioiodine treatment is sufficient for ablation. However, in some cases more than one treatment is required for complete ablation. It has not been proven in the pediatric population if the response to the first ablation therapy has any prognostic value.
Read Also: Doctors Who Specialize In Thyroid
Do All Patients Receive Radioactive Iodine
Radioactive iodine therapy, also referred to as I-131 therapy, is used to treat any thyroid cancer that is left after a total thyroidectomy. This may include either a small amount of cancer remaining in the neck or metastases that cannot be removed with surgery, including cancer that has spread to the lungs. RAI is not used after a lobectomy.
The amount of spread outside of the thyroid gland and to lymph nodes is used to select patients where the benefit from RAI is greater than the risk of treatment. Patients with small tumors and patients with no or minimal evidence of spread to lymph nodes behind the thyroid are considered to be at low-risk and these patients may be followed without receiving RAI ). For patients with evidence of significant spread to tissue next to the thyroid, into lymph nodes or lungs, RAI is administered.
Signs And Symptoms Of Dtc
Most patients with differentiated thyroid cancer do not have any obvious signs or symptoms. In most cases, a thyroid nodule is discovered during a physical exam or through a radiology study for a non-thyroid-related head or neck issue.
When symptoms are present, they may include:
- Feeling a lump in the neck when at rest, lying down, or while eating or drinking
- Change in voice
Also Check: Ttf-1 Positive Thyroid Cancer
How Is Pediatric Thyroid Carcinoma Treated
The most common treatment for thyroid cancer is surgery to remove all or part of the thyroid gland. A thyroid lobectomy is followed by radioactive therapy. Although pediatric thyroid cancer is usually caught at an advanced stage, it has an excellent prognosis, with long-term survival rates of over 95%.
Additional treatments may include:
- Thyroid hormone therapy: an oral medication taken after surgery to replace the hormones that your childs body will no longer be able to produce
- Radioactive iodine: an oral medication that destroys any remaining thyroid tissue after surgery
- External radiation therapy: radiation to the neck or other tissues where the cancer may have spread
- Chemotherapy: an oral or intravenous medication that is used to kill cancer cells
Treatments For Thyroid Cancer
Treatment for thyroid cancer depends on the type of thyroid cancer you have and how far it has spread.
The main treatments are:
- surgery to remove part or all of the thyroid
- radioactive iodine treatment you swallow a radioactive substance that travels through your blood and kills the cancer cells
- external radiotherapy a machine is used to direct beams of radiation at the cancer cells to kill them
- chemotherapy and targeted therapies medicines used to kill cancer cells
After treatment, you’ll have follow-up appointments to check whether the cancer has come back.
Read more about how thyroid cancer is treated.
Don’t Miss: What Is Thyroid Medicine Used For
Testing And Diagnosis Of Mtc
If there is any indication your child may have thyroid cancer, they should be referred to dedicated program, like the Pediatric Thyroid Center at CHOP, that has the experience, expertise and resources to fully evaluate your child.
At Childrens Hospital of Philadelphia, a diagnosis of medullary thyroid cancer begins with a complete medical history and comprehensive physical examination that includes evaluation of the thyroid and the lymph nodes in the neck. Watch CHOP Endocrinologist Andrew J. Bauer, MD, perform a pediatric thyroid exam.
Clinical experts may use a variety of diagnostic tests including:
- Blood test to measure the levels of calcitonin and thyroid-stimulating hormone to determine how well your childs thyroid is working.
- Thyroid ultrasound to learn about the size, number, appearance and location of any thyroid nodules and abnormal lymph nodes.
- Fine-needle aspiration to collect cells from the thyroid, and possibly lymph nodes, to be examined under a microscope.
Treatment For Childhood Thyroid Cancer May Cause Side Effects
For information about side effects that begin during treatment for cancer, see our Side Effects page.
Side effects from cancer treatment that begin after treatment and continue for months or years are called late effects. Late effects of cancer treatment for childhood thyroid cancer may include:
- Physical problems, such as changes in the salivary glands, infection, or trouble breathing.
- Changes in mood, feelings, thinking, learning, or memory.
You May Like: What Is Armour Thyroid Medication
Risks Of Thyroid Surgery
The two most common risks of thyroid surgery include damage to the parathyroid glands or the recurrent laryngeal nerves, structures that are directly attached to the thyroid gland.
- Parathyroid glands: There are four parathyroid glands, two attached to the back of each thyroid lobe. They are about the size of a pencil eraser or pea. The parathyroid glands control the level of calcium in the body. Damage to the parathyroid glands can affect calcium levels and cause significant health risks if left untreated.
- Recurrent laryngeal nerve : The RLN is very thin, about the diameter of a piece of angel hair pasta. The RLN controls the vocal cords and helps protect the airway so food, liquid or other items do not enter the lungs.
The risks of thyroid surgery can be decreased by having the operation performed by an experienced surgical team that completed at least 30 thyroid surgeries per year. The surgeons at the Pediatric Thyroid Center at CHOP perform more than 75 thyroid surgeries a year. The permanent complication rate for thyroid surgery patients at CHOP is less than 2 percent significantly lower than the national average.