Medullary Thyroid Cancer Treatment
A rare type of thyroid cancer called medullary thyroid cancer begins in the thyroid cells that produce a hormone called calcitonin. Radioactive iodine is not effective for these cancers. Targeted therapies such as vandetanib and cabozantinib may be used if the disease recurs after surgery or if it has spread elsewhere in the body . Researchers are looking for better drugs for the treatment of medullary thyroid cancer:
Five Facts About Thyroid Cancer
New Brunswick, N.J., September 1, 2021 The thyroid, a key part of the endocrine system, is a small gland at the base of your neck that produces a hormone that helps control your body’s metabolism. Thyroid cancer occurs when a cell in your thyroid undergoes mutation which cause the cells to grow and multiply rapidly. Amanda M. Laird, MD, FACS, chief of endocrine surgery at Rutgers Cancer Institute of New Jersey and associate professor of surgery at Rutgers Robert Wood Johnson Medical School, shares five facts about thyroid cancer everyone should know.
1. Thyroid cancer is the most common endocrine cancer.
The American Cancer Society estimates that approximately44,280 new cases of thyroid cancer in both men and women will be diagnosed in the U.S. in 2021 with around 2,200 deaths. Fortunately, most types of thyroid cancer are very treatable and survivors live long, healthy lives.
2. While thyroid cancers are common, they may have few or no signs or symptoms.
The most common symptom of thyroid cancer is a painless lump or swelling that develops in the neck. Other symptoms only tend to occur after the condition has reached an advanced stage, which may include unexplained hoarseness or difficulty swallowing that does not go away.
3. There are several types of thyroid cancer.
4. Thyroid cancers occur about three times more often in women than in men.
Papillary Or Follicular Thyroid Cancer
- Stage I — The tumor can be any size. It may have spread to nearby tissues or nearby lymph nodes. But it hasnât spread to other parts of the body.
- Stage II — The tumor is any size. Cancer may have spread to your lymph nodes. It also has spread to other parts of your body, like your lungs or bones.
Read Also: What Is Thyroid Peroxidase Ab
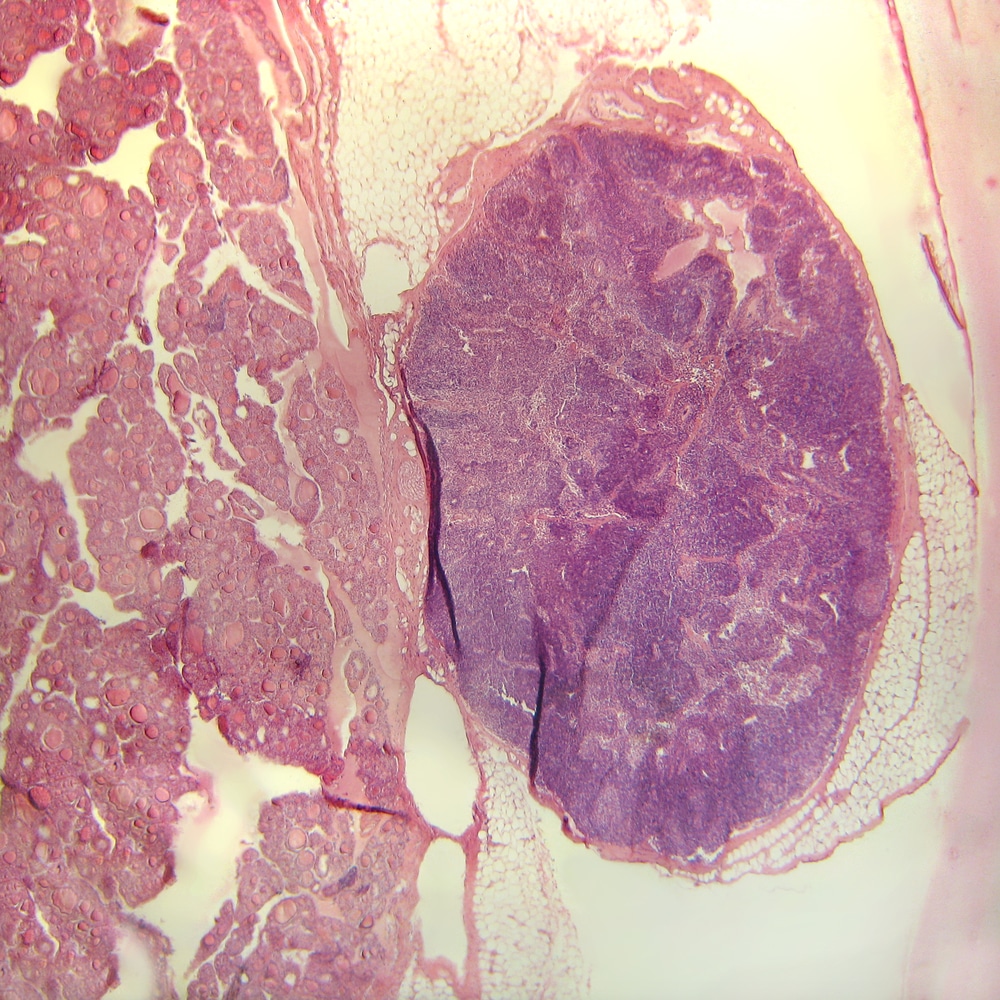
What Are Follicular Thyroid Cancer And Hurthle Cell Carcinoma
Follicular thyroid cancer makes up about 10% of all cases of thyroid cancer.
Follicular thyroid cancer does not often spread to the lymph nodes, but it can spread to other organs, like the liver, lungs, bones, and brain.
Hurthle cell carcinoma is a form of follicular thyroid cancer, and accounts for 3% of all thyroid cancer cases. It is more likely to spread to lymph nodes than follicular thyroid cancer.
Treatments For Thyroid Cancer
Treatment for thyroid cancer depends on the type of thyroid cancer you have and how far it has spread.
The main treatments are:
- surgery to remove part or all of the thyroid
- radioactive iodine treatment you swallow a radioactive substance that travels through your blood and kills the cancer cells
- external radiotherapy a machine is used to direct beams of radiation at the cancer cells to kill them
- chemotherapy and targeted therapies medicines used to kill cancer cells
After treatment, you’ll have follow-up appointments to check whether the cancer has come back.
Read more about how thyroid cancer is treated.
Recommended Reading: How To Reset Thyroid To Burn Fat
Enhancing Healthcare Team Outcomes
Thyroid cancer, as discussed, can have highly varied manifestations, from a clinically indolent low-risk disease that can be managed with only active surveillance to a highly aggressive metastatic disease that needs extensive surgical resection with or without systemic chemotherapy.
Hence, managing a patient with thyroid cancer is a highly individualized process taking into account the patient’s risk of recurrence and preferences . A close collaboration between all interprofessional team members, including but not limited to the thyroid surgeon, the endocrinologist, the pathologist, the radiologist, and possibly the oncologist, plays a vital role in providing the most appropriate treatment for the patient while avoiding overtreatment at the same time. Nursing staff should ensure the patient is involved and comfortable every step of the way, from pre-operative planning to treatment and postoperative monitoring. When pursuing chemotherapy, a specialized oncology pharmacist is also a valuable addition to the interprofessional team. Interprofessional teamwork relies on open communication channels between all team members, and the maintaining of meticulous records so that all professionals involved in the case have access to the same updated patient information and can reach out to other team members if they see anything that requires their attention. This type of interprofessional care coordination combined with open information sharing will yield the best patient outcomes.
Poorly Differentiated And Anaplastic Thyroid Carcinomas
Poorly differentiated thyroid carcinomas are aggressive and are defined histologically by a combination of architectural and high-grade features .62,63 Poorly differentiated thyroid carcinomas represent approximately 6% of thyroid cancers and are associated with a mean survival of 3.2 years. Radioiodine therapy is of limited benefit. Most patients require systemic therapies that are similar to those described for differentiated thyroid carcinomas.
Anaplastic thyroid carcinomas account for approximately 1% of thyroid cancers and are associated with a mean survival of 6 months. They are refractory to radioiodine, and traditional chemotherapy and radiotherapy are of limited benefit.64 Anaplastic thyroid carcinomas probably arise from preexisting differentiated or poorly differentiated thyroid carcinomas and have a high mutation burden.4,55 Although BRAF and RAS are the predominant drivers, anaplastic thyroid carcinomas are characterized by frequent mutations in TP53, the TERT promoter, effectors of the phosphatidylinositol 3-kinase AKTmammalian target of rapamycin pathway, and genes involved in epigenetic regulation, including components of the SWI/SNF complex and histone methyltransferases .55 Mutations in EIF1AX, a component of the translational preinitiation complex, are markedly enriched in poorly differentiated and anaplastic thyroid carcinomas and have a striking pattern of co-occurrence with RAS.
Also Check: Causes Of Thyroid Eye Disease
What Kind Of Support Is Available For Those With Thyroid Cancer
Patients, families, and friends are all affected by a diagnosis of cancer is made. Support is available not only for the patient but for all those who are close to the patient. Hospitals, clinics, and health care professionals’ offices often have specially trained staff to help patients and families address their physical, emotional, and spiritual needs.
It is important for the patient and family to understand the disease, the treatment options, the expected outcomes, and the journey that will occur with cancer. Family members will benefit from being present for provider visits during the diagnosis and treatment, as well as with follow-up appointments. This allows all to be involved in advocating for the patient, since there is so much information to understand and absorb it can be overwhelming.
There are many community resources available as well. The American Cancer Society is a good place to begin. They have local offices and may be contacted online.
How Is Thyroid Cancer Managed Or Treated
Treatments for thyroid cancer depend on the tumor size and whether the cancer has spread. Treatments include:
- Surgery: Surgery is the most common treatment for thyroid cancer. Depending on the tumorâs size and location, a surgeon may remove part of your thyroid gland or all of the gland . The surgeon also removes any nearby lymph nodes where cancer cells have spread.
- Radioiodine therapy: With radioiodine therapy, you swallow a pill or liquid containing a higher dose of radioactive iodine than whatâs used in a diagnostic radioiodine scan. The radioiodine shrinks and destroys the diseased thyroid gland along with cancer cells. This treatment is very safe. Your thyroid gland absorbs almost all of the radioiodine and the rest of your body has minimal radiation exposure.
- Radiation therapy: Radiation kills cancer cells and stops them from growing. External radiation therapy uses a machine to deliver strong beams of energy directly to the tumor site. Internal radiation therapy involves placing radioactive seeds in or around the tumor.
- Chemotherapy: Intravenous or oral chemotherapy drugs kill cancer cells and stops cancer growth. Very few people diagnosed with thyroid cancer will ever need chemotherapy.
- Hormone therapy: This treatment blocks the release of hormones that can cause cancer to spread or come back.
What are the complications of thyroid cancer?
How does thyroid cancer affect pregnancy?
You May Like: Thyroid Peroxidase Antibodies 900 H
Types Of Thyroid Cancer
There are 5 main types of thyroid cancer:
In addition, other types of cancer may start in or around the thyroid gland. For lymphoma in the thyroid, read Cancer.Nets Guide to Non-Hodgkin Lymphoma. For more information on sarcoma in the thyroid, read the Cancer.Net Guide to Sarcoma. For information on a tumor in the nearby parathyroid gland, read Cancer.Nets Guide to Parathyroid Cancer.
Causes Of Thyroid Cancer
Thyroid cancer happens when there’s a change to the DNA inside thyroid cells which causes them to grow uncontrollably and produce a lump.
It’s not usually clear what causes this change, but there are a number of things that can increase your risk.
These include:
- other thyroid conditions, such as an inflamed thyroid or goitre but not an overactive thyroid or underactive thyroid
- a family history of thyroid cancer your risk is higher if a close relative has had thyroid cancer
- radiation exposure in childhood such as radiotherapy
- a bowel condition called familial adenomatous polyposis
- acromegaly a rare condition where the body produces too much growth hormone
You May Like: How Do You Check Thyroid
The Types Of Thyroid Cancer
Different cancers can develop from different cells in the body. According to the National Health Service in the United Kingdom, there are four main types of thyroid cancer, falling under three umbrella categories that are known as differentiated, anaplastic, and medullary:
Papillary and follicular thyroid cancers are known as differentiated thyroid cancers. Differentiated thyroid cancers usually grow slowly over time.
- T describes the size of the tumor
- N signifies the involvement of lymph nodes
- M signifies metastasis, which means the spreading of the cancer cells to other parts of the body
For people under the age of 55, the staging is:
Staging for people over the age of 55 is as follows:
Diagnosing follicular thyroid cancer may include a doctor carrying out the following:
Where Thyroid Cancer Starts
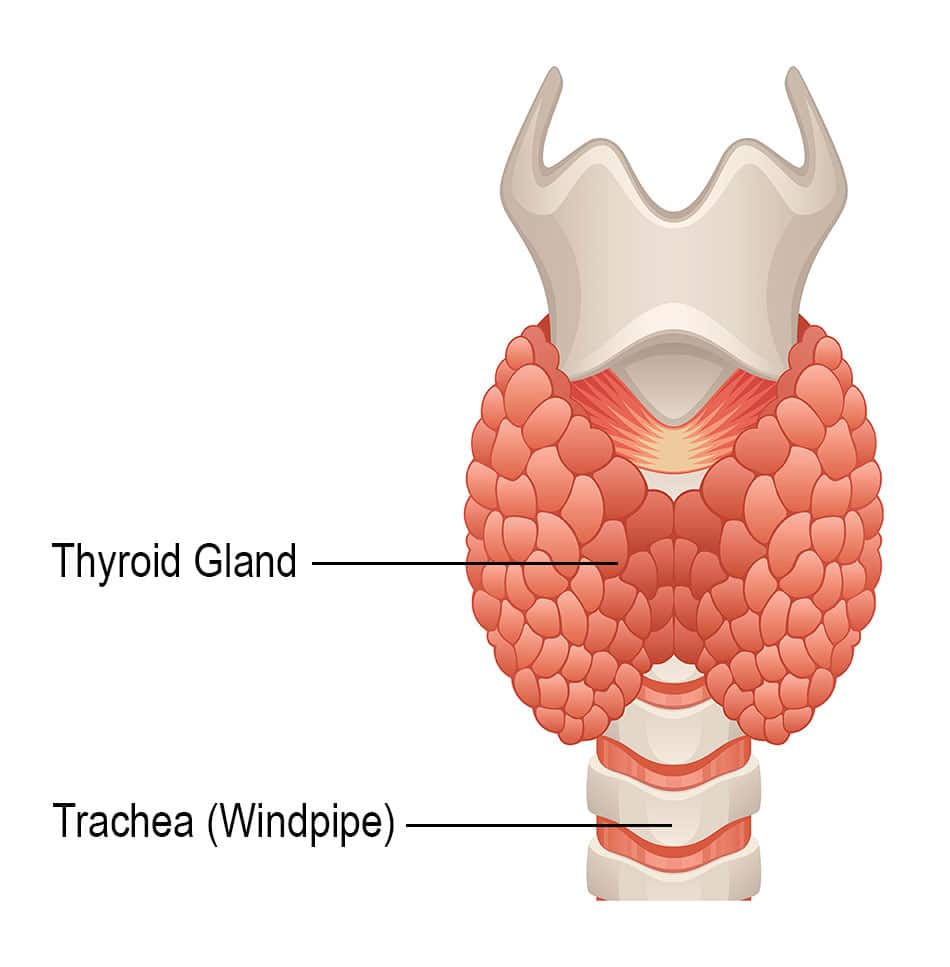
The thyroid gland is in the front part of the neck, below the thyroid cartilage . In most people, the thyroid cannot be seen or felt. It is shaped like a butterfly, with 2 lobes the right lobe and the left lobe joined by a narrow piece of gland called the isthmus.
The thyroid gland has 2 main types of cells:
- Follicular cells use iodine from the blood to make thyroid hormones, which help regulate a persons metabolism. Having too much thyroid hormone can cause a fast or irregular heartbeat, trouble sleeping, nervousness, hunger, weight loss, and a feeling of being too warm. Having too little hormone causes a person to slow down, feel tired, and gain weight. The amount of thyroid hormone released by the thyroid is regulated by the pituitary gland at the base of the brain, which makes a substance called thyroid-stimulating hormone .
- C cells make calcitonin, a hormone that helps control how the body uses calcium.
Other, less common cells in the thyroid gland include immune system cells and supportive cells.
Different cancers develop from each kind of cell. The differences are important because they affect how serious the cancer is and what type of treatment is needed.
Many types of growths and tumors can develop in the thyroid gland. Most of these are benign but others are malignant , which means they can spread into nearby tissues and to other parts of the body.
You May Like: Size Of Thyroid Nodule For Biopsy
Systemic Therapies For Metastatic Radioiodine
Thyroid cancers are often indolent, even when they have metastasized to distant sites. Most physicians reserve systemic therapy for patients who have metastatic disease that is progressing, symptomatic, or in a location that threatens vital structures and is not amenable to localized therapies. Palliative radiotherapy, either alone or concomitant with low-dose chemotherapy, or local therapies may control disease in patients with unresectable regional or metastatic disease.40,41,43 Treatment with bisphosphonates or antireceptor activator of nuclear factor-B ligand antibody may benefit patients who have bone metastases, although the efficacy of the compounds has not been tested in prospective trials.44
The Food and Drug Administration approved two multikinase inhibitors, sorafenib and lenvatinib, for the treatment of patients with radioiodine-refractory metastatic thyroid cancer on the basis of phase 3, prospective, double-blind, randomized, placebo-controlled trials that showed longer progression-free survival .45,46 Although the two drugs have not been compared with each other, lenvatinib appears to have greater efficacy than sorafenib.49 Adverse effects of the two drugs make the maintenance of full-dose therapy a challenge. The effects of the drugs on quality of life and the long-term cumulative toxic effects remain to be fully explored.
Outlook For Thyroid Cancer
Around 9 in every 10 people are alive 5 years after a diagnosis of thyroid cancer. Many of these are cured and will have a normal lifespan.
But the outlook varies depending on the type of thyroid cancer and how early it was diagnosed. At present the outlook is:
- more than 9 in 10 people with papillary carcinoma live at least 5 years after diagnosis
- more than 9 in 10 people with follicular carcinoma live at least 5 years after diagnosis
- more than 7 in 10 men, and around 9 in 10 women with medullary thyroid carcinoma live at least 5 years after diagnosis
- around 1 in 10 people with anaplastic thyroid carcinoma live at least 5 years after diagnosis
Up to 1 in 4 people treated for thyroid cancer are later diagnosed with cancer in another part of the body, such as the lungs or bones, but cancer can often be treated again if this happens.
Page last reviewed: 28 August 2019 Next review due: 28 August 2022
Read Also: Best Supplements For Underactive Thyroid
Whats The Thyroid Cancer Survival Rate
Eight out of 10 people who have thyroid cancer develop the papillary type. Papillary thyroid cancer has a five-year survival rate of almost 100% when the cancer is in their gland . Even when the cancer spreads , the survival rate is close to 80%. This rate means that, on average, youâre about 80% as likely to live for at least five years after diagnosis as someone who doesnât have metastatic papillary thyroid cancer.
Five-year survival rates for other thyroid cancer types include:
- Follicular: Close to 100% for localized around 63% for metastasized.
- Medullary: Close to 100% for localized around 40% for metastasized.
- Anaplastic: Close to 31% for localized 4% for metastasized.
Is thyroid cancer curable?
Yes, most thyroid cancers are curable with treatment, especially if the cancer cells havenât spread to distant parts of your body. If treatment doesnât fully cure thyroid cancer, your healthcare provider can design a treatment plan to destroy as much of the tumor as possible and prevent it from growing back or spreading.
The Tnm Staging System
The American Joint Committee on Cancer created the system thatâs most often used to describe the stages of thyroid cancer. Itâs called the âTNMâ system, and it focuses on these three things:
- T — What is the size and extent of the main, or primary, tumor?
- N — Has the cancer spread to nearby lymph nodes? .
- M — Has the cancer spread, or metastasized, to other areas of the body or organs, namely the lungs, liver, and bones?
After your doctor runs tests to find out what type of thyroid cancer you have, theyâll add a number to each letter listed above. The higher the number, the more advanced is that aspect of the cancer. .
Next, your doctor will group this information into stages. These are represented by the Roman numerals I through IV. For the most advanced cases, the letters âA,â âBâ and âCâ also are used to indicate how far the cancer has spread.
What type of cancer you have, as well as your age, will have some bearing on your stage.
Hereâs what each stage of thyroid cancer means, grouped by types:
You May Like: Braf Mutation In Thyroid Cancer
How Is Anaplastic Thyroid Cancer Treated
Anaplastic thyroid cancer is difficult to treat because it is very aggressive and can spread rapidly within the neck and metastasize to distant parts of the body. It is less predictable than other thyroid cancers however, one thing that all long-term survivors have in common is the sense of urgency in diagnosis and treatment.
It is important to work with a doctor or team of doctors who have experience with anaplastic thyroid cancer. You must be your best advocate. Take a family member or friend to appointments if possible. Take notes. Ask questions. If you are unable to travel to a major medical/ cancer facility with experience, many of the larger, more experienced institutions are happy to advise your local doctors on the best treatment options. Do not be afraid to ask your local doctors to collaborate with experts at more experienced centers on your treatment plan given the rarity of this diagnosis. It is also important to understand the risks and benefits involved with various treatment options.
Anaplastic thyroid cancer does not respond to radioactive iodine therapy or Thyroid Stimulating Hormone suppression, which are commonly used in patients with other forms of differentiated thyroid cancer.
Treatment of anaplastic thyroid cancer, is best done through a multidisciplinary team , and typically consists of combining surgery with external beam radiation and chemotherapy.