Systemic And Locally Injected Glucocorticoids
High-dose systemic glucocorticoids have potent anti-inflammatory and immunosuppressive effects that have been applied successfully for the management of moderate-to-severe and active GO. Intravenous glucocorticoids have been indicated as the first-line treatment in moderate-to-severe and active GO . A proof-of-concept RCT showed a significant improvement of GO outcome in patients treated with i.v. methylprednisolone compared to placebo . Although oral glucocorticoids are effective, glucocorticoids are preferentially administered i.v. as the i.v. route has been shown in RCTs to be more effective and better tolerated . The most common protocol employs a cumulative dose of 4.5 g methylprednisolone, given in 12 weekly infusions . This 4.5 g regimen is very well tolerated and significantly improves QoL . While this regimen is appropriate for most patients, a higher cumulative dose of 7.5 g is reserved for more severe cases within the spectrum of moderate-to-severe and active GO, as the higher dose bears a higher risk of drug-induced adverse events . Safety data suggest that, with the exception of sight-threatening GO, single i.v. doses should not exceed 0.75 g, cumulative doses should be less than 8.0 g per cycle, and consecutive-day therapy should be avoided, because these schedules are associated with a significantly higher rate and clinically relevant glucocorticoid-induced AEs, including liver toxicity and serious cardiovascular AEs .
Mild Active Thyroid Eye Disease
Supportive treatment is the mainstay in mild disease. This involves the maintenance of euthyroidism, strict tobacco avoidance, eye lubrication with drops or ointments, and selenium. Selenium, an antioxidant, when given as 100 mcg twice a day for 6 months, significantly decreased inflammation and improved QoL in patients with mild active TED . Patients with signs of mild TED, per the EUGOGO guidelines, should be referred to centers with both endocrinological and ophthalmological expertise, except for the mildest cases that improve with restoring euthyroidism and topical lubricants .
Severity Of The Disease
Severity is a function of the degree of diplopia, proptosis, and soft-tissue changes, as well as the impact on quality of life . It is categorized by the European Group on Graves Orbitopathy guidelines . Diplopia is classified as absent or transient, inconstant , or constant. Proptosis is measured through a Hertel exophthalmometer, which can be obtained and used by endocrinologists. QoL can be assessed via a validated EUGOGO questionnaire . Mild TED is TED that has a minor impact on QoL with one or more of the following: lid retraction less than 2 mm, mild soft-tissue involvement, proptosis less than 3 mm, and transient or absent diplopia. Moderate to severe TED is disease that is not sight-threatening but has a sufficient impact on the QoL to justify the risks of immunosuppressive or other systemic therapy or rehabilitative surgery . This involves one or more of the following: moderate or severe soft-tissue involvement, proptosis greater than 3 mm, and inconstant or constant diplopia . Finally, sight-threatening disease has either CON or corneal breakdown limiting vision .
You May Like: Thyroid Cancer Brain Metastases Symptoms
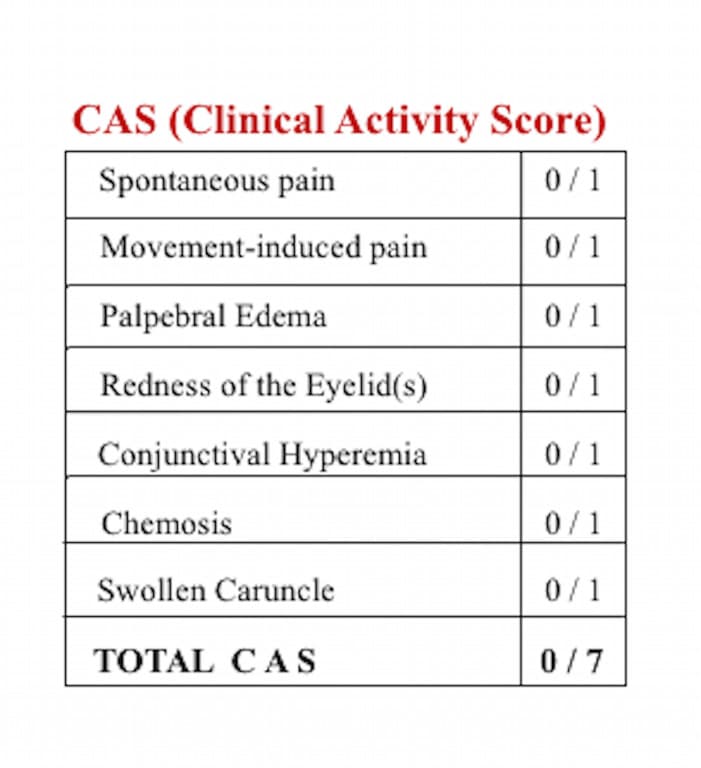
How Is Cas Used To Assess The Severity Of Ted
One point will be given to each of the following symptoms:2,3
- Sudden pain in or around the eye without moving the eye
- Pain when moving the eye
- Swelling of the eyelids
- Redness of the eyeball
- Swelling of the eyeball
- Swelling of the inner corner of the eye
If you have 3 or more symptoms on the CAS 7-point scale, you are considered to have an active case of TED. The higher the number on the scale, the more severe your case may be.2
It is common to have multiple follow-up appointments where CAS is used. This helps your doctor assess whether your symptoms are getting better or worse. These follow-up visits will look at a slightly different set of criteria, such as:2
- Increased eye-bulging
This also allows treatment to be adapted and changed as needed moving forward.2
Clinical And Biochemical Measurements
Bodyweight and height were measured in light clothes and bare feet. Body mass index was calculated as the ratio between weight in kilograms and the square of height in meters . Eyesight was checked using an international visual chart. Intraocular pressure reading was measured with a noncontact tonometer . Proptosis was measured with a Hertel exophthalmometer and recorded as millimeters. The free triiodothyronine , Free thyroxine , and thyroid stimulating hormone were determined with the electro-chemiluminescence method . The thyroid peroxidase antibody , thyroglobulin , and thyroid stimulating receptor antibody were examined using chemiluminescence immunoassay .
Read Also: Thyroid Eye Disease After Thyroidectomy
Patient Characteristics Protocols And Clinical Evaluations
Between October 2009 and May 2010, 16 consecutive patients , with a diagnosis of GO in different phases of thyroid disease, and six normal volunteers were enrolled.
In particular, patients with ocular symptomatology with a proven history of Graves’ thyroid disease or with clinical and laboratory signs of Graves’ disease, ascertained during the first clinical evaluation, were enrolled . Baseline serum thyroid parameters are reported in Table Table1.1. Patients with other orbit diseases such as trauma, optic neuropathy, other inflammatory diseases of unknown origin, previous orbital radiotherapy or surgery, previous immunosuppressive treatments with steroids and antithyroid treatment for more than 12 weeks before MR examination were excluded. All patients gave informed consent and volunteers gave consent to take part in the contrast-enhanced orbital MR studies. The protocol was approved by the local ethical board of our hospital.
Measurement Of Clinical Outcomes
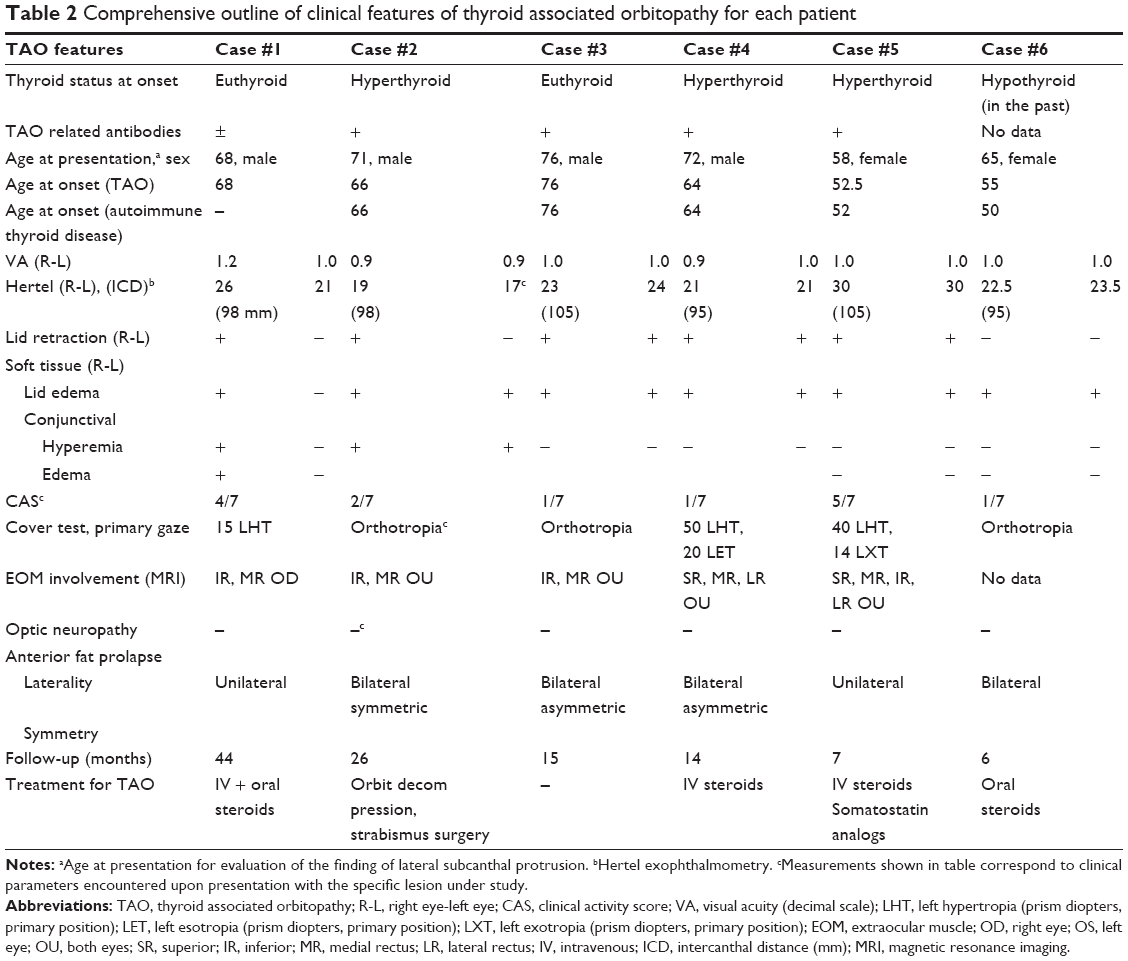
The primary key outcomes of the trials, proptosis, diplopia and CAS response, were evaluated in both eyes to examine differential response from baseline to week 24. Observed data on both placebo and teprotumumab treated patients who met the criteria for asymmetry are reported and compared here for patients with data at both time points.
Proptosis measurements were made using a Hertel exophthalmometer. Changes in diplopia grade were assessed using the Gorman subjective diplopia score . A score of 0 indicates no diplopia intermittent diplopia inconstant diplopia and 3, constant diplopia. An improvement 1 grade is considered as clinically significant. The 7-point CAS was used to measure inflammation. The presence of each of the following symptoms/signs is scored: retrobulbar eye pain, pain on eye movement, eyelid erythema, eyelid swelling, conjunctival redness, chemosis, inflammation of the caruncle or plica. Higher scores indicate more inflammation.
Read Also: How To Get Thyroid Under Control
Study Design And Recruitment Of Participants
After approval from the Institutional Review Board at Yonsei University College of Medicine, informed consent was obtained from all participants. This cross-sectional study included 98 patients with GO who were followed at the Department of Ophthalmology, Yonsei University College of Medicine between January and December 2010. The inclusion criteria were the presence of typical eye symptoms and signs in a patient with autoimmune Graves disease. The patients who have ophthalmic diseases such as cataract, age-related macular degeneration, glaucoma, corneal opacity and so on that could affect the QOL were excluded. Clinical data collected include complete ophthalmic investigations, autoimmune Graves disease progress and medication history, ophthalmological data of visual acuity, intraocular pressure, diplopia tests such as binocular single vision test or Hess screen, and proptosis measurement by Hertel exophthalmometer. All clinical observations and objective measurements were consistently performed by one ophthalmologist .
Inflammation / Congestion And Activity In Ted
Symptoms of ocular and periocular soft tissue inflammation include orbital aching at rest or with movement, and eyelid or conjunctival swelling and redness.
The Clinical Activity Score described and validated by Mourits and the Amsterdam Orbitopathy group assigns one point for each of the following: orbital pain at rest, orbital pain with movement, chemosis, caruncular edema, eyelid edema, conjunctival injection and eyelid injection.
The VISA Inflammatory Score modifies the CAS slightly by widening the grade for chemosis and lid edema from 0-2. Chemosis is graded as 1 if the conjunctiva lies behind the grey line of the lid and as 2 if it extends anterior to the grey line:
Lid edema is graded as 1 if it is present but not causing overhanging of the tissues, and as 2 if it causes a roll in the lid skin including festoons in the lower lid. The worst scores from any of the four eyelids are recorded in the inflammatory score table on the far right section of the table.
The pain score is based on the patients report of deep orbit discomfort rather than ocular surface irritation . The additional grading scores for chemosis and lid edema allow for documentation of more subtle changes in inflammatory features between visits. An additional point is assigned for diurnal variation of symptoms, to reflect the variability in congestion typically seen during the active phase.
Recommended Reading: Home Thyroid Test Kit Walgreens
Orbital/ophthalmic Surgery In The Treatment Of Go
In the active phase of GO, decompression surgery is indicated in patients with severe exposure keratopathy and, as second-line treatment, in patients with DON not responding to i.v. glucocorticoids. Local treatment can be used in the same phase as temporary measures to shield the cornea for superficial damages or to correct extreme corneal thinning, thus decreasing risks of spontaneous eyeball perforation or perforation in the course of subsequent decompression surgery. In the post-inflammatory, inactive phase, residual disfigurements can be treated by a combination of decompression, ophthalmic plastic, and strabismus surgery .
Management Of Thyroid Dysfunction
The baseline thyroid status of the patients is shown in Tables 3 and 4. Patients who were euthyroid at their first MDTED appointment were the result of well controlled thyroid disease or euthyroid GD. Out of 166 patients who had TSH antibody titre measurement, 75.9% had a positive titre status. In our cohort, 23.7% patients had a recurrence of hyperthyroidism 66.7% had this before and 33.3% after their first attendance at the MDTED clinics. One hundred and three patients were discharged from the MDTED clinics during the study period and 76.7% were biochemically euthyroid at discharge.
Table 3 Patient baseline characteristics by disease activity at presentation.
Table 4 Endocrinological characteristics of the cohort by disease activity.
Also Check: Lab Tests For Thyroid Problems
What Is Exophthalmometry
Another common method in evaluating TED is to use exophthalmometry. This procedure looks at whether a person has proptosis, a condition when the eyes bulge and protrude out of the eye sockets.3
Proptosis is a very clear, visible sign of TED and is common among active and more severe cases. It is measured by an exophthalmometer . This is a handheld tool that measures the distance from the outer edges of the eye socket to the uppermost point of the cornea.2,3
Table 1 Tao Evaluation
- Intraocular pressure
- Adnexal examination
- Orbital ultrasound to assess extraocular muscle size
- Orbital CT without contrast or MRI to assess extraocular muscle size, orbital fat and proptosis
You can make the diagnosis of TAO based on presenting ocular signs and symptoms. Changes in appearance and exposure symptoms are the most common early findings in TAO.9 Other symptoms are vague and often attributed to normal aging, especially in middle-aged women with eyelid swelling that is worse in the morning.12
The most common sign in TAO is lid retraction, which occurs in 82% of patients.13 This may be due to increased sympathetic tone, overaction of the levator and superior rectus muscles to compensate for inferior rectus restriction, or inflammation and scarring of the levator complex .
The second most common sign is proptosis , which is caused by expansion of the orbital fat, muscles or both . Proptosis can be measured with an exophthalmometer. Values greater than 18mm to 20mm for Caucasians, 16mm to 18mm for Asians and 20mm to 22mm for African-Americans suggest proptosis. Asymmetry of 2mm or greater also suggests proptosis.14,15 If a clinician does not have an exophthalmometer, orbital CT scans can evaluate the amount of proptosis as well.
| Fig. 3. Upper eyelid retraction and proptosis in a patient with orbital congestion in the active phase. |
You May Like: Why Does Armour Thyroid Cost So Much
Management Of Go During Viral Pandemic
Patients with mild GO should receive the usual local treatment and should be urged to quit smoking to prevent progression of GO . As to moderate-to-severe and active GO, glucocorticoids and other immunosuppressive agents could make patients more susceptible to infections . Discontinuation of long-term glucocorticoid treatment may be associated with adrenal failure, which, in turn, increases the risk of developing infections and related mortality, likely including COVID-19 . Nevertheless, unless immunized or having had COVID, all of us have no immunity to COVID, so adding immunosuppression will not increase that risk. Furthermore, dexamethasone or methylprednisolone or tocilizumab has now become the standard of care for COVID . Also, it is now clear that very high-dose steroids used in COVID does not cause adrenal suppression, and normal adrenal function was observed in patients who survived COVID-19 Infection . In line with this, withdrawal of i.v. glucocorticoid treatment in GO patients is not associated with adrenal failure .
Health And Lifestyle Habits
The health of your immediate family members may offer important clues about your current health. Your doctor may ask questions about family medical history for this reason.
When asked about your lifestyle habits, be open and honest with your doctor. Habits like smoking significantly increase the risk of developing TED.3,4
Recommended Reading: What Happens If You Dont Take Your Thyroid Medication
Clinical And Biochemical Characteristics Of The Active Inactive Tao Patients And Controls
All the TAO patients enrolled have not received the anti-TAO treatment including glucocorticoid therapy, radiotherapy, or surgical decompression surgery. Most patients had symmetrical activity of GO, except one had unilateral active GO. As shown in Table , compared with the control group, the overall TAO patients had significantly elevated serum levels of FT3 and thyroid autoantibodies , as well as abnormal ocular signs . Compared with the inactive TAO patients, the active TAO patients were older and consumed more tobacco. Also, the intraocular pressure and degree of exophthalmos were much worse in the active TAO patients. There were no significant differences in terms of sex, disease duration, BMI, thyroid function, and thyroid autoantibodies between the inactive and active groups.
Table 1 General Characteristics of subjects
Horizon Therapeutics Plc Completes Enrollment For Phase 4 Trial Of Tepezza In Adults With Chronic/low Clinical Activity Score Thyroid Eye Disease
— Topline results expected in second quarter of 2023 —
DUBLIN, September 29, 2022—-Horizon Therapeutics plc announced that it has completed enrollment of its Phase 4 clinical trial evaluating TEPEZZA for the treatment of Thyroid Eye Disease in patients with a low Clinical Activity Score , also known as the TEPEZZA Chronic TED trial. CAS is a tool designed to evaluate inflammatory signs and symptoms that are often associated with TED.1 Topline results are expected in the second quarter of 2023.
TED is a serious, progressive and potentially vision-threatening rare autoimmune disease. Symptoms of TED may include dry eyes and grittiness redness, swelling and excessive tearing eyelid retraction proptosis pressure and/or pain behind the eyes and diplopia . TEPEZZA was approved by the U.S. Food and Drug Administration in January 2020 as the first and only medicine for Thyroid Eye Disease.
This randomized, double-masked, placebo-controlled, parallel-group, multicenter trial is evaluating the efficacy, safety and tolerability of TEPEZZA compared to placebo in treating TED patients with a low CAS , two to 10 years since eye symptom onset, and non-worsening proptosis for at least a year. Adult participants who met the trial eligibility criteria were randomized in a 2:1 ratio to receive an infusion of either TEPEZZA or placebo, 10 mg/kg for the first infusion and 20 mg/kg for the remaining seven infusions, once every three weeks, for a total of eight infusions.
About TEPEZZA
Also Check: Gaia Herbs Thyroid Support Reviews
Clinical Presentation Of Ted
About 90% of patients with TED also have some thyroid dysfunction – usually the thyroid is overactive , but occasionally the thyroid is underactive . Most times, the diagnosis of TED and diagnosis of a thyroid dysfunction occur within the same year. Patients who are diagnosed with TED but have no known thyroid dysfunction should see their primary care physician for an evaluation of their thyroid function.
The disease course for TED involves 2 phases – active and stable. In the active phase there is active swelling and inflammation. This presents as redness in and around the eye, eye pain with or without eye movement, as well as swelling around the eyes and eyelids. The active phase of TED involves a waxing/waning period of these symptoms, and can last months to years. On average, the active phase of TED lasts about 1 year for non-smokers, and 2-3 years for smokers . The active phase of TED spontaneously transitions to the stable phase, but can recur. Active TED has a recurrence rate of about 5-10%, but is less likely to recur after 18 months in the stable phase.
Figure 3. Active vs. Stable TED. Active TED is characterized by signs of inflammation . TED activity waxes and wanes, and usually transitions to stable TED within 1-3 years.
Figure 4. Rundle’s curve. As seen in the representation of TED activity over time in Rundle’s curve, initiating therapy early is crucial to diminish the overall severity of the chronic disease.
Assessing The Severity Of Thyroid Eye Disease
- Reactions 0 reactions
For people with thyroid eye disease , assessing the severity during its active phase is key. This is because TED only responds to treatment when a person has active symptoms, not when symptoms are inactive.1
The earlier your treatment plan can begin, the better your quality of life will be. The most common way to assess the severity of TED is to use the Clinical Activity Score, also known as the CAS 7-point scale.2
Read Also: Hair Loss From Thyroid Disease
Table 3 Management Of Thyroid Eye Disease
Disease Stage Refractory
- Steroid-sparing immunomodulators
When using CAS, note that severe disease complications, such as dysthyroid optic neuropathy, are still possible with low CAS scores, and patients with high CAS scores may have long-standing congestive changes that are unresponsive to any immunotherapy, requiring mechanical surgical decompression.
Latent. After the active phase plateaus, the patient enters the quiescent burn-out phase. This latent, chronic fibrotic phase presents with similar clinical findings as the active inflammatory phase but does not have many of the inflammatory signs seen during the active phase .23 These patients require frequent follow-up, as reactivation of inflammation can occur in 5% to 10% of patients over their lifetime.24