Less Common Way Of Increasing Your Tsh
If you are not able to have the rhTSH injection, your doctor may advise you to stop taking your thyroid hormones . This is because thyroid hormone replacement stops your body from making TSH. You usually stop taking them for a few weeks before and during your treatment. This allows your body to make its own TSH. Your doctor or nurse will tell you when to stop taking them. It is important to stop taking thyroid hormones when you are told to, or the RAI treatment may not work as well as it should.
While you are not taking your thyroid hormones, you will have the symptoms of thyroid hormone withdrawal. These are likely to include:
- tiredness , weakness and a lack of energy
These symptoms should stop when you start taking the thyroid hormone tablets again, but it can take some time.
Are There Long Term Risks Of I
In general, RAI is a safe and effective treatment for the thyroid disorders mentioned above. Hypothyroidism is a common side effect of RAI for hyperthyroidism and always seen after RAI for thyroid cancer. This is usually easily treated with thyroid hormone replacement . Some studies suggest a slight increase in thyroid cancers may be seen after RAI treatment for hyperthyroidism. Loss of taste and dry mouth due to salivary gland damage may be seen. The use of lemon drops, vitamin C or sour stimulation to potentially decrease the exposure of the salivary glands to RAI is controversial and should be discussed with your physician. Importantly, once you have been treated with RAI, regular medical follow-up is lifelong.
Clearing The Radioactive Iodine From Your Body
Some of the radioactive iodine will be taken up by your thyroid cells, but there will be some left over. Most of the extra radioactive iodine will leave your body through your urine , and smaller amounts will leave your body in your saliva , sweat, and bowel movements .
Follow these guidelines to help the radioactive iodine leave your body quickly.
- Drink lots of liquids. Starting right after your treatment, try to drink at least 1 cup of low-iodine liquid every hour while youre awake. Keep doing this for 2 to 3 days after your treatment. You dont have to wake up at night to drink liquids.
- Your urine will be radioactive so urinate as much as you can to empty your bladder. Try not to get urine outside of the toilet. If you do get urine outside of the toilet, wear gloves and clean up it up with an all-purpose cleaning disinfectant. If you normally stand while urinating, sit for 2 days after your treatment unless your healthcare provider gives you other instructions. This is so you can avoid getting urine anywhere but the toilet. Try to urinate every time you feel the urge instead of holding it in your bladder.
- Your bowel movements will also be radioactive. Go to the bathroom as much as you can so your bowel movements dont stay in your colon.
- If youre often constipated , ask your doctor about taking laxatives before your treatment. If you dont have a bowel movement within 24 hours after your treatment, call your doctor.
Don’t Miss: What Is An Overactive Thyroid Called
How Does Radioactive Iodine Treat Hyperthyroidism
Your thyroid, a butterfly-shaped gland located in the lower front of your neck, produces hormones that regulate your bodys metabolism and other functions. Hyperthyroidism speeds up the bodys processes causing nervousness and anxiety, rapid heartbeat, missed or light menstrual periods, sleep problems, hand tremors and other problems.
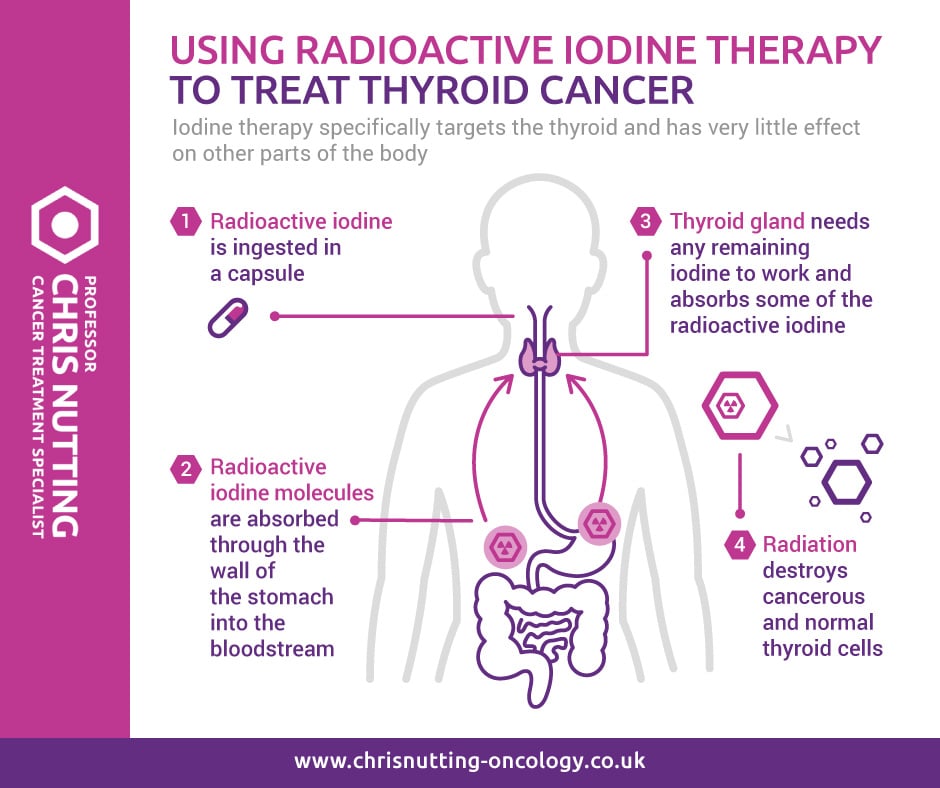
The thyroid gland needs iodine to make these hormones. The thyroid is the most efficient organ at concentrating iodine. RAI treats hyperthyroidism by damaging or destroying thyroid cells through radiation.
RAI is taken in an oral capsule form. You dont need to be hospitalized unless the dose is very high, which is rarely needed. You will be prompted to drink lots of water after taking the pill to flush the remaining radioactive iodine out of your system.
Most patients need only one dose before their hyperthyroidism is resolved, which may take a few weeks to several months. If your symptoms are still there after six months, you may have to receive a second dose.
Preparation Of A Hurthle Cell Cancer Patient For Radioactive Iodine Treatment
Hurthle cell cancer patients must be taken off of levothyroxine thyroid hormone for a minimum of four weeks, taken off of liothyrionine thyroid hormone for a minimum of two weeks, or receive a medication which is TSH . Additionally, hurthle cell cancer patients must be on a low iodine diet for a minimum of four weeks to starve their body of iodine. Those patients which have undergone CAT scans with intravenous contrast must wait until their blood iodine levels have been adequately decreased . Note, a desire to treat with radioactive iodine should never prevent the use of necessary CAT scans for the evaluation of a hurthle cell cancer patient.
- Dry mouth and or eyes
- Narrowing of the drainage duct of the eyes tears leading to excessive tearing down the cheek
- Swelling in your cheeks from inflammation or damage to the saliva producing glands
- Short term changes to taste and smell
- Lowered testosterone levels in males
- Change in periods in women
You May Like: Location Of The Thyroid Gland
Breastfeeding And Radioactive Iodine Therapy
Radioactive iodine can collect in breast tissue with milk in it. To prevent having radioactive iodine collect in your breast after your treatment, youll need to stop breastfeeding or pumping breast milk at least 6 to 12 weeks before your treatment.
You wont be able to continue breastfeeding after your treatment because your breast milk can expose your baby to radiation. If you have any questions about breastfeeding and your treatment, talk with your doctor or call the Department of Medical Physics at .
Maximizing The Effectiveness Of Radioactive Iodine Therapy
Radioactive iodine therapy for thyroid cancer is most effective in people who have high levels of thyroid-stimulating hormone, or TSH. This hormone is produced by the pituitary gland, which is located at the base of the brain and produces many hormones. TSH tells the thyroid to absorb iodine, which is then converted to thyroxine. The thyroids ability to absorb iodine is important for the success of radioactive iodine therapy.
If youve had surgery to remove part or all of the thyroid, your doctor may wait a few weeks before prescribing a replacement thyroid hormone. During that time, you experience whats known as thyroid hormone withdrawal, which makes the pituitary excrete more TSH. Excess thyroid-stimulating hormone is necessary for the success of radioactive iodine therapy.
Another way your doctor may try to increase the effectiveness of radioactive iodine therapy is to give you an injection of a medication called recombinant human thyroid hormonethyroid-stimulating hormone made in a laboratory. This injection is given for two days before radioactive iodine therapy begins. The medication elevates thyroid-stimulating hormone levels enough to make the radioactive iodine therapy as effective as thyroid hormone withdrawal.
When radioactive iodine therapy is being considered for thyroid cancer, the body must be depleted of inorganic iodine, so the levels of thyroid-stimulating hormone increase, helping with the effectiveness of radioactive iodine therapy.
You May Like: Who Is The Specialist For Thyroid
Radioactive Iodine Therapy For Thyroid Cancer
Your thyroid gland absorbs nearly all of the iodine in your body. Because of this, radioactive iodine can be used to treat thyroid cancer. The RAI collects mainly in thyroid cells, where the radiation can destroy the thyroid gland and any other thyroid cells that take up iodine, with little effect on the rest of your body. The radiation dose used here is much stronger than the one used in radioiodine scans, which are described in Tests for Thyroid Cancer.
This treatment can be used to ablate any thyroid tissue not removed by surgery or to treat some types of thyroid cancer that have spread to lymph nodes and other parts of the body.
Radioactive iodine therapy helps people live longer if they have papillary or follicular thyroid cancer that has spread to the neck or other body parts, and it is now standard practice in such cases. But the benefits of RAI therapy are less clear for people with small cancers of the thyroid gland that do not seem to have spread, which can often be removed completely with surgery. Discuss your risks and benefits of RAI therapy with your doctor. Radioactive iodine therapy cannot be used to treat anaplastic and medullary thyroid carcinomas because these types of cancer do not take up iodine.
When Do You Have Radioactive Iodine
You might have radioactive iodine treatment:
- after surgery, to kill any cancer cells that may have been left behind
- to treat thyroid cancer that has spread
- to treat thyroid cancer that has come back after it was first treated
You may only need to have this treatment once. But it can be repeated every 3 months if needed, until there is no sign of any thyroid cancer on your scans.
Also Check: How To Regulate Your Thyroid
Radioactive Iodine Treatment For Papillary Thyroid Cancer
The mechanism of how RAI Treatment works to treat thyroid cancer was not discovered until years following its use to treat papillary thyroid cancers. We now know today that papillary thyroid cancers can possess a type of key hole on the surface of their cell called a symporter that allows iodine to be taken into the cell. Under normal circumstances, iodine is taken up by normal thyroid cells in the process of producing the bodys thyroid hormone. Although papillary thyroid cancer rarely produces thyroid hormone itself, it frequently maintains this iodine symporter and ability to take up iodine. In the treatment of papillary thyroid cancer, this can be taken advantage of by having the patient swallow an iodine pill that has been radioactively charged.
The papillary thyroid cancer patient swallows a radioactive iodine form of iodine called iodine 131 in a liquid or pill form. The RAI is absorbed through digestion and circulated throughout the body in bloodstream. Papillary thyroid cancer cells can pick up the radioactive iodine wherever they are located in the body. Once taken into the papillary thyroid cancer cells, the radioactive iodine delivers a local radiation treatment in the area where the iodine is concentrated.
How Is The Procedure Performed
Hyperthyroidism treatment is almost always done on an outpatient basis because the dose required is relatively small.
The radioiodine I-131 is swallowed in a single capsule or liquid dose and is quickly absorbed into the bloodstream in the gastrointestinal tract. It is concentrated from the blood by the thyroid gland, where it begins destroying the gland’s cells. Although the radioactivity remains in the thyroid for some time, it is greatly diminished within a few days. The effect of this treatment on the thyroid gland usually takes between one and three months to develop. Maximum benefit occurs three to six months after treatment. Usually, a single dose is successful in treating hyperthyroidism. However, rarely, a second treatment is necessary. A third treatment is very rarely necessary.
Recommended Reading: Treating Thyroid Cancer Without Surgery
Help Getting Through Cancer Treatment
People with cancer need support and information, no matter what stage of illness they may be in. Knowing all of your options and finding the resources you need will help you make informed decisions about your care.
Whether you are thinking about treatment, getting treatment, or not being treated at all, you can still get supportive care to help with pain or other symptoms. Communicating with your cancer care team is important so you understand your diagnosis, what treatment is recommended, and ways to maintain or improve your quality of life.
Different types of programs and support services may be helpful, and can be an important part of your care. These might include nursing or social work services, financial aid, nutritional advice, rehab, or spiritual help.
The American Cancer Society also has programs and services including rides to treatment, lodging, and more to help you get through treatment. Call our National Cancer Information Center at 1-800-227-2345 and speak with one of our trained specialists.
Physical Emotional And Social Effects Of Cancer
Thyroid cancer and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative care or supportive care. It is an important part of your care that is included along with treatments intended to slow, stop, or eliminate the cancer.
Palliative care focuses on improving how you feel during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of cancer, may receive this type of care. And it often works best when it is started right after a cancer diagnosis. People who receive palliative care along with treatment for the cancer often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. You may also receive palliative treatments similar to those meant to get rid of the cancer, such as chemotherapy, surgery, or radiation therapy.
Learn more about the importance of tracking side effects in another part of this guide. Learn more about palliative care in a separate section of this website.
You May Like: What Happens If Thyroid Cancer Goes Untreated
Before Your Radioactive Iodine Treatment
For your treatment to work, one of the hormone levels in your body needs to be high. This hormone is called thyroid stimulating hormone or TSH. A high level of TSH helps any thyroid cancer cells in the body to take up radioactive iodine.
To increase the levels of TSH, your doctor will ask you to do one of the following:
- have an injection of a man-made TSH called recombinant human TSH once a day for 2 days
- stop taking your thyroid hormone tablets a few weeks before treatment
Your healthcare team will explain what you need to do and what is going to happen. They will also let you know when to re-start your hormone tablets if they have asked you to stop taking them.
Preparation Of A Papillary Thyroid Cancer Patient For Radioactive Iodine Treatment
Papillary thyroid cancer patients must be taken off of levothyroxine thyroid hormone for a minimum of four weeks, taken off of liothyrionine thyroid hormone for a minimum of two weeks, or receive a medication which is TSH . Additionally, papillary thyroid cancer patients must be on a low iodine diet for a minimum of four weeks to starve their body of iodine. Those patients which have undergone CAT scans with intravenous contrast must wait until their blood iodine levels have been adequately decreased . Note, a desire to treat with radioactive iodine should never prevent the use of necessary CAT scans for the evaluation of a papillary thyroid cancer patient.
The potential risks of RAI treatment include:
- Dry mouth and or eyes
- Narrowing of the drainage duct of the eyes tears leading to excessive tearing down the cheek
- Swelling in your cheeks from inflammation or damage to the saliva producing glands
- Short term changes to taste and smell
- Lowered testosterone levels in males
- Change in periods in women
Also Check: What Can I Do To Help My Underactive Thyroid
New Research Casts Doubt On A Cornerstone Of Thyroid Cancer Treatment
For decades, radiation has been a cornerstone of thyroid cancer care. But it may soon be phased out entirely for many thyroid tumors as emerging research casts doubt on whether it benefits patients.
A study published Wednesday in the New England Journal of Medicine suggests that surgery alone might be sufficient to cure the lowest-risk thyroid cancers, and that follow-up treatment with radioactive iodine offers no additional benefit for these patients.
Its almost a given that once patients have their thyroid taken out, they get radioactive iodine, said David Cooper, an endocrinologist at the Johns Hopkins University School of Medicine. Recently, people have been wondering whether it really does what its supposed to, whether its potential harms are worth the potential benefits.
Part of the trouble with answering that question is that low doses of radioactive iodine, which are typically given for low-risk thyroid cancer, arent all that bad. Classically, radioactive iodine might cause nausea, discomfort, or in some cases, damage to the salivary glands, but many patients wont even experience that, Cooper said.
The main burden is that the procedure costs time and money, and brings the remote risk that the radiation itself could cause another cancer.
For low-risk we felt there might not be any need for it, she said. So we decided to do another study to see if radioiodine therapy was even useful.
Neck Pain And Swelling
Radiation thyroiditis with swelling and thyroid pain occurs 3 to 7 days after RAI therapy. Generally, this risk is very low after near-total or total thyroidectomy without extensive neck metastases.38 A painless swelling of the neck has been described that occurs within 48 hours after the RAI treatment. This edema is believed to a hypersensitivity reaction in the tissues surrounding the thyroid. Both painful and painless neck swelling may be treated with corticosteroids, if necessary.
Also Check: Thyroid Eye Disease After Thyroidectomy
Thinking About Taking Part In A Clinical Trial
Clinical trials are carefully controlled research studies that are done to get a closer look at promising new treatments or procedures. Clinical trials are one way to get state-of-the art cancer treatment. In some cases they may be the only way to get access to newer treatments. They are also the best way for doctors to learn better methods to treat cancer. Still, they’re not right for everyone.
If you would like to learn more about clinical trials that might be right for you, start by asking your doctor if your clinic or hospital conducts clinical trials.